Association of NT-Pro BNP within Hospital Outcome of Anterior STEMI at Tertiary Care Hospital, Chattogram, Bangladesh
Mohammad Humayun Kabir*1, Nayeema Tasnim2, Shantanu3
1Lecturer, Dept. of Biochemistry, Holy Family Red Crescent Medical College, Dhaka, Bangladesh
2Professor, Dept. of Biochemistry, Chattogram Medical College, Chattogram, Bangladesh
3Assistant Professor, Dept. of Biochemistry, Institute of Applied Health Sciences (IAHS), Chattogram, Bangladesh
*Corresponding author: Mohammad Humayun Kabir, Lecturer, Dept. of Biochemistry, Holy Family Red Crescent Medical College, Dhaka, Bangladesh
Received: 07 July 2025; Accepted: 10 July 2025; Published: 07 August 2025
Article Information
Citation: Mohammad Humayun Kabir, Nayeema Tasnim, Shantanu. Association of NT-Pro BNP with in Hospital Outcome of Anterior STEMI at Tertiary Care Hospital, Chattogram, Bangladesh. Fortune Journal of Health Sciences. 8 (2025): 743-748.
Share at FacebookAbstract
Background: BNP (Brain natriuretic peptide) is released from cardiac myocytes due to their stretching, volume overload and high filling pressure. All of these actions result in high wall stress which initiates the release of pro-BNP, precursor of BNP. It cleaves first to pro-BNP, then to the biologically active BNP and the inactive amino-terminal fragment, N-terminal pro hormone of BNP, NT-pro BNP.
Objective: This study aims to observe the association of NT-pro BNP with anterior STEMI patients.
Methods: A cross-sectional comparative study was conducted in the Department of Biochemistry of Chittagong Medical College and with the collaboration of the Department of Cardiology at Chittagong Medical College Hospital by non-probability purposive sampling. 59 patients having STEMI (myocardial infarction) with heart failure and 59 patients having STEMI (myocardial infarction) without heart failure were investigated. Important variables in this study used were age, gender, MI (myocardial infarction), heart failure and serum NT-pro BNP, and ejection fraction.
Result: There was a significant mean difference in NT-pro BNP, serum creatinine, BMI and eGFR between MI with heart failure and anterior STEMI without heart failure. A significant negative correlation was observed between NT-pro BNP and ejection fraction in patients with anterior STEMI with heart failure. Significant negative correlation between NT-pro BNP and eGFR in anterior STEMI with heart failure. Among the study population, all the 59 patients of anterior STEMI with HF have increased NT-pro BNP, and 58 patients of anterior STEMI without HF have increased NT-pro BNP. The eGFR, hypertension group, diabetes, and BMI statistically significantly predict the increased NT-pro BNP in STEMI with heart failure.
Conclusion: Elevated NT-pro BNP levels in STEMI patients are strongly associated with the development of heart failure. It serves as a key biomarker for early risk assessment and prognosis. High levels indicate greater myocardial stress and worse cardiac outcomes.
Keywords
NT-Pro BNP, Anterior STEMI, Heart Failure, Without Heart Failure, Outcome, Bangladesh
Article Details
Introduction
During the last decade, B-type-natriuretic peptides have rapidly transitioned from laboratory research to practical clinical application. Originally, they were brought into clinical use as a means of diagnosing heart failure.1 Later, their independent prognostic value has been demonstrated, particularly in relation to mortality and heart failure.1 There has been a strong association between heart failure and myocardial infarction. When considered on their own, heart failure has a significantly worse prognosis than myocardial infarction.2 It has been estimated that the proportion of chronic heart failure patients are 20–35%.3 NT-proBNP is the N-terminal fragment of pro BNP, which is the precursor of BNP and is a high-molecular-weight molecule that is biologically inactive. The primary origin of NT-pro BNP is the heart muscle cell. In this context, NT-pro BNP is produced by cleaving it from its precursor and released in equimolar amounts along with BNP. NT-pro BNP is found in high amounts in the blood of humans and remains unchanged in whole blood.4 Diastolic dysfunction of the left ventricle (DDLV) is believed to represent the initial manifestation of myocardial functional impairment. Alterations in the myocardial structure, including an increase in the thickness of the left ventricular mass, have been documented. There may be a resultant increase in ventricular volumes and impairments in contractility.5With the progression of cardiac dysfunction, the production and release of cardiac natriuretic peptides increase in heart failure. Hence, it has been suggested that elevated levels of B-type natriuretic peptide (BNP) and/or N-terminal pro BNP (NT-pro BNP) could serve as an indicator of symptomatic ventricular dysfunction. Furthermore, regardless of the severity of left ventricular dysfunction, patients with a history of myocardial infarction and cardiomyopathy have higher levels of blood BNP or NT-pro BNP.6 The Framingham study demonstrated that people with high plasma BNP levels are more likely to develop Congestive Heart Failure.7 It is, therefore, possible that NT-pro BNP levels may serve as a useful marker of cardiovascular risk in patients with heart failure.8 These findings are consistent with the known activation of pro BNP synthesis in response to mechanical and neurohumoral stimulation of the heart, as well as the increased secretion of BNP from hypertrophied and failing ventricles, resulting in a strong association between BNP and left ventricular systolic dysfunction. Recent studies have demonstrated elevated NT-pro BNP concentrations in experimental LV dysfunction and after acute myocardial infarction (MI).4 The high negative predictive value indicates that NT-pro BNP might be particularly useful for the exclusion of impaired LV function, and a normal test result would allow us to virtually rule out significant LV dysfunction. Furthermore, the sensitivity of NT-pro BNP was sufficient to biochemically identify the majority of subjects with LV dysfunction, and this provided valuable information, even without taking into account further clinical information. Specifically, three fourths of subjects with significant LV dysfunction (EF<35%) were identified at the given cut-points. Because biochemical markers for LV dysfunction are not yet established in current practice, subjects may still often remain misdiagnosed.4 Non-invasive cardiac imaging like 2D Echocardiogram and MRI of the heart is essential for diagnosis, evaluation and management of heart failure, but these are time-consuming and less acceptable. However, circulating NT-pro BNP is highly sensitive to heart failure with preserved and depressed ejection fraction in asymptomatic patients.9The N- terminal pro-B-type natriuretic peptide (NT-pro BNP) level in the early stages of heart failure (HF).4 Therefore, this study will try to observe the association of NT-pro BNP with anterior STEMI.
Objectives
- To observe the distribution of NT-pro BNP levels in patients with anterior STEMI with heart failure
- To observe the distribution of NT-pro BNP levels among the study population
- To find out the correlation of NT-pro BNP levels with ejection fraction, and eGFR among the study population
- To analyse and compare the mean NT-pro BNP levels between patients with anterior STEMI with heart failure and anterior STEMI without heart failure
- To see the association of elevated NT-pro BNP levels of patients with anterior STEMI with heart failure
Materials and Methods
Study design: Cross-sectional comparative study.
Study period: This study was conducted from July, 2023 to June, 2024.
Place of study: Department of Cardiology, Chittagong Medical College Hospital and Department of Biochemistry, Chittagong Medical College, Bangladesh.
Permission for the study: Ethical approval for this research protocol was obtained from the Ethical Review Committee of Chittagong Medical College, Memo No: 59.27.0000.013.19. PG.009.2024/1082.
Study population:
Group A: Patients having anterior STEMI with heart failure.
Group B: Patients having anterior STEMI without heart failure.
Sample technique: Non-probability purposive sampling.
Sample size: The sample size will be calculated by the following formula:
Sample size: The sample size will be calculated by the following formula
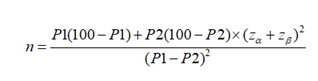
Where,
n= required sample in each group.
P1 = Prevalence of myocardial infarction with reduced ejection fraction in heart failure (Group A) (from the previous study)
P2= Prevalence of myocardial infarction with normal ejection fraction in heart failure (Group B) (from the previous study)
P1 − P2 = difference of proportion between Group A and Group B (from the previous study)
Zα= Z-value of standard normal deviate at a given level of significance
Zβ = Z-value of standard normal deviate at a given power.
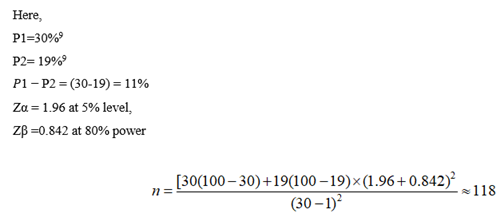
Here, a total of 118 subjects were taken.
Of which 59 subjects with STEMI with heart failure and 59 subjects with STEMI without heart failure as a comparison group were taken to test the hypothesis.
Statistical analysis and presentation of the results
All the data were compiled into master sheet, processed and analyzed using Microsoft Excel and IBM-SPSS (Statistical package for social science) version 26 for Windows. The mean, standard deviation, and standard error of means were calculated for each parameter and finally, the values had computed within the two study groups by applying the student t-test. Statistical inference was based on 95% confidence interval (CI) and “p” value <0.05 was considered statistically significant. Categorical variables were presented as frequency (percentages) or proportions. Pearson’s correlation (r) test was used to observe the correlation between continuous variables. The summarized data was presented in the form of tables and figures.
Results and observations
Table I: Distribution of age and gender among the study population (n=118)
|
Variable |
MI with HF (59) |
MI without HF (59) |
|
|
|
Mean ±SD |
59.81±11.01 |
57.94±9.53 |
|
Age |
Range |
38-91 |
40-85 |
|
|
Male |
55 (93.2%) |
43 (72.9%) |
|
Gender |
Female |
04 (6.8%) |
16 (27.1%) |
Comment: Table I shows the mean age of patients in anterior STEMI with heart failure is 59.81±11.01 and anterior STEMI without heart failure is 57.94±9.53. The minimum and maximum age of anterior STEMI with heart failure is 38 & 91 respectively. The minimum and maximum age of anterior STEMI without heart failure is 40 & 85 respectively. Among the study population, 93.2% are male & 6.8% are female in anterior STEMI with heart failure. 72.9% are male and 27.1% are female in anterior STEMI without heart failure.
Table II: Independent sample t-test to see the association of parameters between MI with heart failure and anterior STEMI without heart failure (n=118)
|
MI with HF |
MI without HF |
||
|
Variable |
(Mean ± SEM) |
(Mean ± SEM) |
p-value |
|
NT-Pro BNP |
10477.16±1351.78 |
506.64±31.85 |
<0.001* |
|
Serum creatinine |
1.24±0.022 |
0.85±0.018 |
<0.001* |
|
BMI |
23.17±0.46 |
19.26±0.32 |
<0.001* |
|
eGFR |
61.52±1.51 |
92.5±2.9 |
<0.001* |
Comment: Table II shows that there is a significant mean difference in NT- pro BNP, serum creatinine, BMI and eGFR between anterior STEMI with heart failure and anterior STEMI without heart failure.
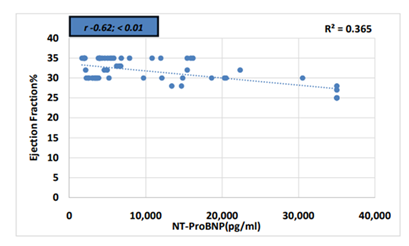
Comment: There is a significant negative correlation between NT-pro BNP and ejection fraction in patients with anterior STEMI with heart failure.
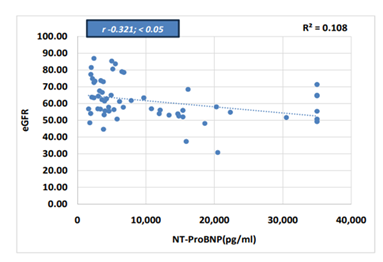
Comment: There is a significant negative correlation between NT-Pro BNP and eGFR in anterior STEMI with heart failure.
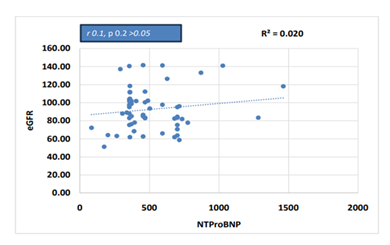
Comment: There is no correlation between NT-pro BNP and eGFR in anterior STEMI without heart failure.
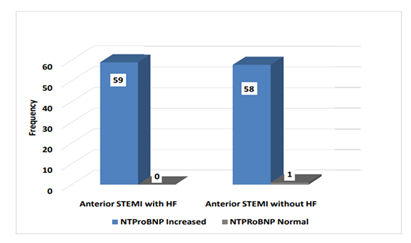
Comment: Among the study population, all the 59 patients of anterior STEMI with HF have increased NT-pro BNP, and 58 patients of anterior STEMI without HF have increased NT-pro BNP.
Table III: Multiple linear regression analysis prediction of increased NT-pro BNP by different factors
|
ANOVAa |
||||||||||||
|
|
|
|
|
|
|
|||||||
|
Model |
Sum of Squares |
df |
Mean Square |
F |
Sig. |
|||||||
|
1 |
Regression |
2839117341 |
6 |
473186224 |
8.271 |
.000b |
||||||
|
Residual |
6350086639 |
111 |
57207987.7 |
|||||||||
|
Total |
9189203980 |
117 |
||||||||||
|
a. Dependent Variable: VAR00001 |
||||||||||||
|
b. Predictors: (Constant), BMI, HTN, Age, DM, Gender Group, eGFR |
||||||||||||
|
Unstandardized Coefficients |
Standardized Coefficients |
|||||||||||
|
B |
Std. Error |
Beta |
t |
Sig. |
||||||||
|
(Constant) |
10843.855 |
6309.537 |
1.719 |
0.088 |
||||||||
|
Age |
54.425 |
68.177 |
0.065 |
0.798 |
0.426 |
|||||||
|
Gender group |
-3060.475 |
1996.438 |
-0.13 |
-1.533 |
0.128 |
|||||||
|
eGFR |
-100.857 |
30.026 |
-0.295 |
-3.359 |
0.001* |
|||||||
|
HTN group |
5280.809 |
1450.492 |
0.296 |
3.641 |
0.000* |
|||||||
|
DM group |
340.616 |
1456.738 |
0.019 |
0.234 |
0.816 |
|||||||
|
BMI group |
6389.821 |
2398.141 |
0.219 |
2.664 |
0.009* |
|||||||
|
a. Dependent Variable: NT-pro BNP category (STEMI with heart failure and STEMI without heart failure) |
||||||||||||
Comment: The regression model predicts the dependent variable is highly significant. This indicates the statistical significance of the regression model that was run. Here, p < 0.0005, which is less than 0.05, and indicates that, overall, the eGFR, hypertension group, diabetes, BMI statistically significantly predicts the increased NT-pro BNP in anterior STEMI with heart failure (table-III).
Discussion
BNP is produced by ventricular cardiomyocytes in particular when the heart is subjected to an excessive volume or pressure strain. Under typical circumstances, the levels of circulating BNP and NT-pro BNP are typically within the normal range. Nevertheless, in individuals who have heart failure, these levels significantly increase as a compensatory measure to return to normal haemodynamics.10 In this study there was a significant mean difference in NT- Pro BNP, between MI with heart failure and Anterior STEMI without heart failure (Table II). During the first phase of acute myocardial infarction (AMI), there is a rapidly loss in both ventricular diastolic and systolic function. This is caused by myocardial ischaemia at the site of the infarction, which leads to the rapid release of B-type natriuretic peptide (BNP). As a result, there is a large rise in the concentration of N-terminal pro-BNP (NT-pro BNP) in the serum. Thus, NT-pro BNP levels may serve as an indicator of ventricular stress, infarct size, and left ventricular dysfunction.11-14 There was a significant negative correlation between NT-Pro BNP and ejection fraction in patients with anterior STEMI with heart failure (Figure 1).The predictive values of NT-pro BNP at given cut-points indicating marginal or significant LV dysfunction were studied by (Luchner, A. et al. 2002)4 showed that using NT-pro BNP testing may effectively rule out LV dysfunction in an outpatient population. This method has a strong negative predictive value and has amazing sensitivity and specificity. The substantial negative predictive value suggests that NT-proBNP might be very valuable in ruling out impaired LV function, and a normal test result would effectively exclude the possibility of major LV dysfunction. Moreover, the NT-proBNP sensitivity was enough to biochemically detect most individuals with LV failure, thus offering significant information, independent of additional clinical data. There was a significant negative correlation between NT-pro BNP and eGFR in anterior STEMI with heart failure (Figure 2). There was no correlation between NT-Pro BNP and eGFR in anterior STEMI without heart failure (Figure 3). NT-pro BNP is an important predictor of mortality but is inversely related to estimated glomerular filtration rate (eGFR) (Ozkan, B. et al. 2023)15 found that for every drop of 15 units in eGFR, the level of NT-pro BNP was 4.3 times greater for eGFR less than 30, 1.7 times higher for eGFR between 30 and 60, 1.4 times higher for eGFR between 61 and 90, and 1.1 times higher for eGFR between 91 and 120 mL/min/1.73 m2. There was a significant mean difference in NT-Pro BNP, serum creatinine, eGFR between MI with heart failure and anterior STEMI with heart failure (Table II). (Luchner et al. in 2002)4, revealed that NT-pro BNP levels were considerably higher in patients with renal dysfunction and those who had previously had a myocardial infarction. Furthermore, the levels of NT-pro BNP grew progressively and significantly in inverse relation to the ejection fraction. A significantly elevated level of NT-pro BNP was seen in a small number of individuals with poor kidney function, despite the lack of left ventricular dysfunction. This elevation was also observed in individuals with both mild and severe left ventricular dysfunction. Among the study population, all the 59 patients of anterior STEMI with HF have increased NT- pro BNP, and 58 patients of anterior STEMI without HF have increased NT-pro BNP (Figure 4). The regression model identifies the association of the dependent variable significantly well. Here, p < 0.05, and indicates that, overall, the eGFR, Hypertension group, Diabetes, and BMI statistically significantly predict the Increased NT-Pro BNP (Table III).
Conclusion
Elevated levels of NT-pro BNP is strongly associated with both ST-elevation myocardial infarction (STEMI) and heart failure. This biomarker reflects the extent of myocardial stress and damage, making it a valuable tool in diagnosing and managing these conditions. In STEMI, NT- pro BNP levels can help estimate the severity of myocardial injury and guide therapeutic interventions. In heart failure, elevated NT-pro BNP concentrations are indicative of the degree of cardiac dysfunction and can assist in monitoring disease progression and response to treatment.
References
- Radosavljevic-Radovanovic M, Radovanovic N, Vasiljevic Z, et al. Usefulness of NT-proBNP in the follow-up of patients after myocardial infarction. J Med Biochem 35 (2016): 158–65.
- Luchner A, Hengstenberg C, Löwel H, et al. N- terminal pro-brain natriuretic peptide after myocardial infarction: A marker of cardio-renal function. Hypertension 39 (2002): 99–104
- Cowie MR, Struthers AD, Wood DA, et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet 350 (1997): 1349-53.
- Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347 (2002): 161-7.
- McKelvie RS, Moe GW, Ezekowitz JA, et al. The 2012 Canadian Cardiovascular Society heart failure management guidelines update: focus on acute and chronic heart failure. Can J Cardiol 29 (2013): 168–81.
- Oremus M, McKelvie R, Don-Wauchope A, et al. A systematic review of BNP and NT-proBNP in the management of hDemaio AR, Otgontuyaeart failure: overview and methods. Heart Fail Rev 19 (2014): 413–9.
- Di Angelantonio E, Chowdhury R, Sarwar N, et al. B-type natriuretic peptides and cardiovascular risk: systematic review and meta-analysis of 40 prospective studies: Systematic review and meta-analysis of 40 prospective studies. Circulation 120 (2009): 2177–87.
- Doust JA, Pietrzak E, Dobson A, et al. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review BMJ 330 (2005).
- Vesbianu D, Vesbianu C, Bernstein P, et al. Plasma brain natriuretic peptide-an independent predictor of mortality and re hospitalization in congestive heart failure-a meta- analysis. World Heart J 1 (2008): 349–54.
- Hall C. NT-Pro BNP: the mechanism behind the marker. J Card Fail 11 (2005): S81–S83.
- Wang Y, Zhou S, Yang F, et al. Treatment-Related Adverse Events of PD-1 and PD-L1 Inhibitors in Clinical Trials: A Systematic Review and Meta-analysis. JAMA Oncol 5 (2019): 1008-1019.
- Qin Z, Du Y, Zhou Q, et al. NT-proBNP and Major Adverse Cardiovascular Events in Patients with ST-Segment Elevation Myocardial Infarction Who Received Primary Percutaneous Coronary Intervention: A Prospective Cohort Study. Cardiol Res Pract (2021): 9943668.
- Goetze JP, Gore A, Moller CH, et al. Acute myocardial hypoxia increases BNP gene expression. FASEB J 18 (2004): 1928– 1930.
- Alzaabi MA, Abdelsalam A, Alhammadi M, et al. Evaluating Biomarkers as Tools for Early Detection and Prognosis of Heart Failure: A Comprehensive Review. Card Fail Rev 10 (2024): e06.
- Ozkan B, Grams ME, Coresh J, et al. Associations of N-terminal pro-B-type natriuretic peptide, estimated glomerular filtration rate, and mortality in US adults. Am Heart J 264 (2023): 49–58.