Contraception in Teens and Young adults with Congenital Heart Disease
Raffaella Marzullo*,1, Gabriella Gaudieri1, Alessandro Capestro2, Mario Giordano1, Gianpiero Gaio1, Carmela Morelli1, Fiorella Fratta1, Fortuna Del Gaizo1, Assunta Merola3, Ludovica Spinelli Barrile4, Giuseppe Limongelli5, Berardo Sarubbi3, Maria Giovanna Russo6
1Pediatric Cardiology, University of Campania 'Luigi Vanvitelli', Former, Second University of Naples, Monaldi Hospital-AORN Ospedali dei Colli, Naples, Italy
2Pediatric and Congenital Cardiology and Cardiac Surgery, University Hospital "Ospedali Riuniti", Ancona, Italy
3Adult Congenital Heart Diseases Unit, AORN dei Colli, Monaldi Hospital, Naples, Italy
4Pediatric Cardiology, University of Campania 'Luigi Vanvitelli', Former Second University of Naples, Monaldi Hospital-AORN Ospedali dei Colli, Naples, Italy
5Inherited and Rare Cardiovascular Disease Unit, Department of Translational Medical Sciences, University of Campania "Luigi Vanvitelli”, Naples, Italy
6Pediatric Cardiology, University of Campania 'Luigi Vanvitelli', Former Second University of Naples, Monaldi Hospital-AORN Ospedali dei Colli, Naples, Italy
*Corresponding Author: Raffaella Marzullo, Pediatric Cardiology, University of Campania 'Luigi Vanvitelli', Former Second University of Naples, Monaldi Hospital-AORN Ospedali dei Colli, Via Leonardo Bianchi 1, 80131, Naples, Italy.
Received: 07 October 2025; Accepted: 14 October 2025; Published: 27 October 2025
Article Information
Citation: Raffaella Marzullo, Gabriella Gaudieri, Alessandro Capestro, Mario Giordano, Gianpiero Gaio, Carmela Morelli, Fiorella Fratta, Fortuna Del Gaizo, Assunta Merola, Ludovica Spinelli Barrile, Giuseppe Limongelli, Berardo Sarubbi, Maria Giovanna Russo. Contraception in Teens and Young adults with Congenital Heart Disease, Fortune Journal of Health Sciences. 8 (2025): 975-984
Share at FacebookAbstract
Reproductive and sexual health are an important part of overall wellness for adolescent and young adults with Congenital Heart Diseases (CHDs). Good sexual health encompasses not only the physical well-being but also social, mental and emotional aspects. In this setting, medical care and comprehensive sexuality education, which gives them information for preventing unintended pregnancies, unsafe abortions, sexually transmitted infections and to support good sexual choices is crucial This document provides a comprehensive summary of contraceptive options and aims to be used as a resource to guide cardiovascular specialists on contraception in the context of care of CHD patients.
Keywords
Contraceptions, Congenital Heart diseases, Sexual education, Pregancy, Couseling
Article Details
Introduction
Both medical and surgical advances in the treatment of Congenital Heart Diseases (CHDs) have increased the survival rates for the affected patients across all age groups. The demographic shift in the population living with CHDs documented that almost 90% of patients now achieve adulthood (1,2). Of these, adolescents and emerging adults in transition age represent 15% to 20% of the overall population with CHDs (3). Adolescence is the age during which major developments of sexuality takes place involving not only bodily changes, but also emotional maturity, sexual orientation, relationship skills, and sexual behaviors. Accordingly, there is an increasing need to discuss about the sexuality and reproductive health with adolescents and young adults with CHDs focusing specifically on contraception and preconception (1). In this article, we discusse how to approach to sex-related topics and how prescribe contraceptive issues among the different needs of patient with CHDs to support the sexual well-being, prevent unplanned pregnancies and encourage safe contraceptive methods.
Adolescence and Reproductive Health
Adolescence is a critical phase of transition from childhood to adulthood marked by significant physical, social, and emotional change (4, 5). The hormonal influences result in the onset of puberty leading to significant anatomic and neuropsychological changes. Body and mind undergo so many transformations in a very small time and to reach a new balance with itself and the world around can be hard. New emotions bursting in daily life: every feeling is lived at its highest intensity, making every new experience exciting and worth to be lived. Sexuality is a natural modality to discover the new world: in this stage of life, the adolescent experiences and explores sexual feelings, discovering its sexual identity and its sexual orientation. New drives and desires cause sexual sensation seeking and sexual curiosity. However, the exposure to idealized and/or sexualized social stereotypes and the misconception of own invulnerability contributes to imprudent sexual withdrawals resulting in potentially dangerous situations.
Thus, sexual and reproductive health is today a matter of concern among youth people. The worries are related to a wide range of risky sexual behaviors such as unprotected sex, non-consensual experiences, high rates of Sexually Transmitted Diseases (STDs) and unintended pregnancy that may trigger negative effect on mental health of the teens and may promote their stigmatization from society (6).
Sexual Activity in Teens and Young adults with Congenital Heart Disease
Timing of sexual debut is heavily influenced by individual, familiar, social and environmental circumstances. In a world that runs fast, young people grow-up faster and live precociously new experiences. Large population-based sexual health studies have all reported a decrease in the age of sexual debut among adolescents and youth over the most recent decades. In the western word, the median age of menarche is around 12-13 years and the median age of the first intercourse is around 17 years for both women and men with ≈30% of youth sexually active before 15 years (7-9). Early sexual initiation increases the risk of STDs and unintended pregnancies, but also it makes youth people vulnerable to psychiatric disorders including depression, substance use, eating disorders, antisocial personality, and suicide (9).
Sexual habits of patients with CHDs are similar to general population. They are equally sexually active as their healthy counterparts. The number of partners since being sexually active not differ between patients with CHDs and those without (10). Current trends shown that the use of contraceptive methods at initial sexual activity is increased among teens like as the use of highly effective contraceptive method is raised among teen females. However, there are adolescents with CHDs still do not use any method of contraception at first intercourse or do not continue to use contraception regularly (10,11). It is estimated that one in four sexually active adolescent has a STDs (8) The incidence of STDs is similar in CHDs patients compared to non CHDs patients, although the rate of Herpes manifestations is higher than in those with CHDs (10).
Unintended pregnancy in adolescents with CHDs.
Although the adolescent birth rate declines worldwide, the number of adolescent mothers remain high, especially among those with poor education or low economic status. It was estimated that approximately 50% of adolescent pregnancies were unintended leading serious health, social and economic consequences for the young woman, her family, and society. Adolescent pregnancy contributes in addition to maternal and child mortality (6). The use of effective contraceptive methods is main strategy to prevent pregnancy in this age group. However, the availability of contraception for adolescents changes across the regions. The cost of contraception may be an important barriers to use for teens. While the short-acting contraception is relatively affordable, the long-acting methods may be more expensive. In addition, the lack of knowledge on where to obtain them and how to correctly use them may create barriers for teens seeking contraception.
Contraceptives methods in Teens and Young adults with Congenital Heart Disease
Girls and young women with CHDs experience contraceptive methods later than general population (12). It is estimated that approximately 76% of sexually active women with CHDs use contraceptives (13). However, more than half of women with CHDs not received specific informations about contraceptive or reproductive counseling respect to their cardiac condition. Among those who reported discussing sexual activity with a physician, only 47% received counseling prior to their first sexual intercourse (14). Among the women who had never discussed contraception, 80% were sexually active (13). Women with CHDs were more likely to receive counselling than women with other medical diagnoses. Specifically, women with complex CHD were more likely to receive contraceptive counseling compared to those with less complex (8,15). The gynecologists were the primary source for these informations while the Adult Congenital Heart Disease (ACHD) specialists provide counseling in less than 50% of cases (8,16).
In the digital era, internet represents the principal source of contraceptive informations for the teens (17). The condom is the most common used method of contraception (38%), followed by oral contraceptives (30%) and withdrawal (11%) (12). It suggests that women with CHDs are still using less effective contraceptive methods. In addition, 10% of patients receives inappropriate contraceptive methods prescription according to their specific CHDs with 53% of them reported a history of use (13). Subsequently, based on these data, it is not surprising that 45% of pregnancies in CHDs women are unexpected (13). Limited and poor-quality data exist on the safety of contraceptive methods in CHDs patients (16,18-20). Patients with more complex CHDs using Oral Contraceptives (OCs) may be a higher risk of thrombotic events compared to general population (13). Specifically, patient with Fontan, Eisemenger syndrome or Transposition of the great arteries using OCs present a major risk compered to non users (13). One of these studies reported also that the thromboembolic risk in complex CHD is more than mild CHD (13). Finally, no studies found endocarditis among Intrauterine Device (IUD) users (16-18).
Contraceptive Methods
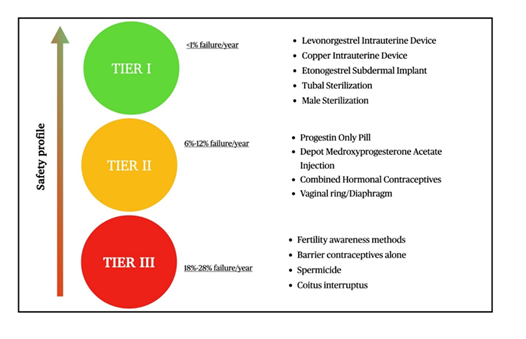
Contraceptive methods can be classified into 3 tiers according to their 1 year-failure rates in current use (Fig.1). The tiers provide guidance to physicians to make informed decisions regarding the safety of contraceptive use in the setting of the individual patient’s specific cardiovascular conditions.
Tier 1: Highly Effective Methods
Intrauterine contraceptive devices
Intrauterine devices (IUDs) are small flexible devices that are inserted into the uterus. There are 2 type of IUDs: the Copper-based IUD (also called non-hormonal) and progesterone-containing IUD (hormonal). The non-hormonal device induces an inflammatory reaction that prevent sperm implantation. They represent a contraceptive choice specifically for women with contraindications to hormones. They can be used for up to 10 years with a typical use 1-year failure rate of 0.8% (21,22). Spotting or frequent bleedings are common in users during the first 3 to 6 months, but they are usually self-limited. This aspect should be taken in consideration specifically for women on anti-platelet or anticoagulant agents for which should be consider other contraceptives. Other possible side effects include tender breasts, headaches, skin changes and mood changes. The hormonal IUDs contain Levonorgestrel. Its local release induces endometrial atrophy and cervical mucus plug. It can stay in place for up to 3-6 years with a typical-use 1-year failure rates of 0.2% to 0.9%. There are not report of myocardial infarction, venous thromboembolism and stroke associated with the use of these hormonal devices. Hormonal IUDs should be considered particularly in patients with heavy menstrual cycle to reduce the bleeding and/or in patients on anti-platelet or anticoagulant agents (amenorrhea is reported in up to 20% of 52-mg levonorgestrel-IUD users) (21, 22).
All type of IUDs can be placed in the outpatient setting. However, for patients in which vasovagal response may have a strong hemodynamic impact (such as with Fontan circulation, Pulmonary Hypertension and severe left obstructive diseases), it would be better to implant in hospital where the clinics should be prompt to treat the possible complications. Finally, the risk of endocarditis with IUD insertion is very low so that the prophylactic antibiotics are generally not recommended (13, 23). IUDs (both copper and hormonal) do not give protection from STDs for which is indicated to use barrier protection such as condoms (21,22).
Implants
The sub-dermal implant is a small Etonogestrel-releasing rod placed subcutaneously in the inner non dominant upper arm. Ovulation inhibition is achieved by direct action on endometrium but also indirectly through the suppression of the hypothalamic-pituitary-ovarian axis. It provides an effective long acting protection for up to 3 years with a typical use failure rate of 0.05%. Its immediate reversibility doesn’t impact on future fertility (22,24). The easy use and the high efficacy a makes the Etonogestrel implant a valid option for adolescents with all CHDs. However, their acceptance and continuation are sometimes affected by side effects. Irregular bleeding is the most common side effect. It is documented especially in patients in the younger age and with lower BMI (25,26). Similarly, the weight gain is more frequent among adolescent and young adult patients (27). Acne is also reported in two-thirds of the users (28). Other side effects include mood changes and headaches.
Sterilization
It is a permanent form of birth control and the most effective contraception method. Male sterilization strategy consist in vasectomy, a surgical procedure based on the ligation and interruption of the vas deferens preventing the passage of sperm at the time of ejaculation.It is usually performed in-office under local anesthesia. Complications happen in 1-2% of cases and may include hematoma, infection and chronic pain syndrome. The estimated rate of failure in the first year after vasectomy is 0,15% , lower than that of female sterilization (30). In addition to efficacy, vasectomy provides a more cost-conscious and safer alternative compared to female sterilization. Despite these advantage, this method of sterilization is still underutilized in the United States in favor to tubal sterilization (29, 30)
Female sterilization works to prevent pregnancies through the occlusion or the discontinuation of the fallopian tube. There are many surgical sterilization procedures including salpingectomy, tubal ligation, and hysteroscopic occlusion of the fallopian tubes that may be used. Laparoscopic approach is usually used for both bilateral salpingectomy and tubal interruption; this latter may be obtained applying clips, silicone ribber rings or using electrocoagulation. However, the procedural steps of laparotomic approach include general anesthesia, positive pressure ventilation and carbon dioxide peritoneal insufflation (to enhance the surgeon’s view of anatomic structures). The net effect of preoperative management in most situations is a decrease in cardiac output and in restriction of the pulmonary flow, making these procedures unsuitable for patients with complex CHDs like Fontan circulation, severe pulmonary artery hypertension or Eisenmenger’s syndrome. In these settings, if necessary, laparoscopic surgery can be performed with minimal abdominal inflation under regional or local anesthesia. Alternatively, hysteroscopic sterilization with micro inserts in the fallopian tubes can be safety considered (31). Overall, the risk of procedural complications are lower with hysteroscopic than laparoscopic sterilization although this latter is associated with better gynecological outcomes (31).
Tier II: Moderately Effective Methods
Combined hormonal contraceptives (CHCs)
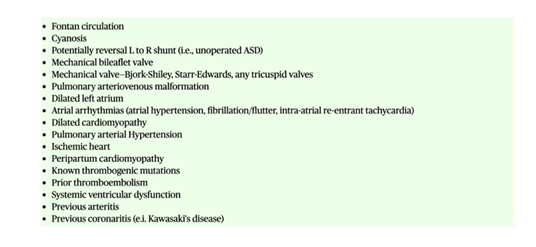
CHCs contain both estrogen and a progestin and are the most common forms of prescribed contraceptives in teens. They are available in different forms (pill, transdermal patch, vaginal ring) Each of these carries a typical-use 1-year failure rate of 9%, which can be as low as 0.3% with perfect use. (13). They work by stopping the ovulation via feedback in the hypothalamic-pituitary-ovarian axis and thickening cervical mucus. These methods are reversible and can be used by patients of all ages (32). The most important risks of CHCs are related to both arterial and venous thrombotic events. The thrombogenicity is due at least in part to multiple changes in clotting factors mediated by estrogen component. The thromboembolic risk seems not to change according the doses of ethinyl estradiol and not vary among the pill, patch, and the ring and the different pill formulations (22). This aspect requires caution in prescription especially in young CHDs’s woman s at increased risk of thromboembolism (4,22) (Fig.2) Additionally, adolescent patients with concomitant thromboembolic predisposing factors (such as smoking and obesity) should be counseled about the increased risk of events and should be encouraged to change their life style . However, it should be noted, that the risk of thromboembolism in patients taken CHC methods is lower than the risk of pregnancy-associated events (22).
Finally, CHCs may predispose to higher risk of arrhythmia ( 33) in patients who are already at increased risk of atrial and ventricular arrhythmias.
Progesterone-only preparations.
Progesterone only contraception is available in different formulations (pills and injections). It works preventing implantation by the reduction of endometrial receptivity and by the inhibition of ovulation. Progestin-only pills include Norethindrone, Norgestrel, and Drospirenone formulations. Daily adherence influences the failure rate that is estimated at 1% with perfect use and 9% with typical use. The benefits of progestin-only contraceptive pills include ease of initiation and discontinuation, fertility return within 1 cycle, safety profile, and minimal effect on hemostatic parameters (34). Thus, they are indicated for all women with CHDs advised against estrogen use such as with history of thromboembolic disorders or hypertension. Additionally, these formulations are the best contraceptive methods in young breastfeeding women because they do not reduce the milk production. Irregular bleeding is the most common side effect reported in the users.
Depot Medroxyprogesterone Acetate (DMPA) is an injectable progestin available in intramuscular (150 mg) and subcutaneous (104 mg) formulations with no difference in effectiveness or adverse effects. Each injection of DMPA provides protection against pregnancy for 12 weeks. Many users, including adolescents, choose this contraceptive method because its high effectiveness with 0.2–0.3% unintended pregnancy rate in the first year for perfect use and 6% for typical use. The leading disadvantages of DMPA are menstrual irregularities, spotting and prolonged bleeding (up to 12 months after the last dose). Delay in fertility is also documented after the final dose. As such, DMPA may be not the best contraceptive method for women wanting to become pregnant in the near future (22,32,35). Finally, DMPA injections are associated with a reduction in bone mineral density. Thus, alternative methods of contraception should be not considered as first in patient aged under 18 years or of any age with risk factors for osteoporosis.
Tier III: Poorly Effective Methods
Barrier forms of contraception
Barrier contraceptives include condoms, diaphragms, cervical caps, and contraceptive sponges. The main function of these methods is preventing unintended pregnancy. The efficacy depends on their correct and consistent use. Thus, they are not recommended for stand alone use in women with high risk of serious morbidity or mortality related to pregnancy (1, 13). In most cases, the barrier forma of contraception can be used in combination with different contraceptive methods to achieve maximum effectiveness (1, 13). Anyway, the use of some barrier methods of contraception, specifically condoms and dental dams, should be encouraged to prevent STDs (1).
Emergency contraception
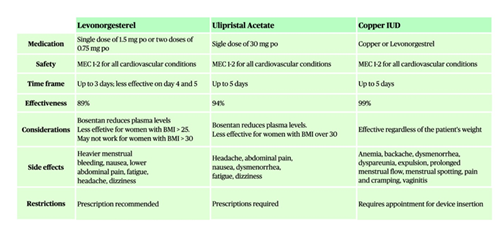
Emergency contraception (EC) is used to prevent pregnancy after unprotected intercourse or a failed contraception. It works effectively when taken between 3-5 days after the sex. EC options include: oral emergency contraceptive and intrauterine device. The available methods, in order of increasing effectiveness, with recommended timing of use has been summarized in Fig.3. Intrauterine device is the most effective type and it may be particularly appropriate for women with CHDs requiring a highly effective, long-acting, and reversible contraceptive method. There are 2 different types: copper IUDs and hormonal IUDs. Some people prefer a hormonal IUD over the copper IUD because it can reduce menstrual bleeding and discomfort.
In women with known thrombophilic disorders or history of thromboembolic events, either progestin only pills and selective progesterone receptor modulators can be used without increased risk of thrombosis (1,36,37) . Enhanced anticoagulant effect of warfarin has been reported in patients taken high-dose levonorgestrel for emergency contraception (38). Consequently, it may be better consider intrauterine devices for post-coital contraception in a women taking warfarin. Additionally, it is important to consider the potential drug-drug interactions among Levonorgestrel (LNG) and Ulipristal acetate (UPA) and Bosentan. In fact, all those drugs works as CYP3A4 inducers. Thus, in patients treated with the endothelin receptor antagonist, the blood levels of those emergency contraceptive drugs, may be reduce and be less effective, increasing the risk of unintended pregnancy. There are no age-specific differences in the use of EC between adolescents and adults and there is not an increased risk of adverse events in adolescents compared to adults. Notably, EC will not interfere with an established pregnancy.
Non-contraceptive Benefits
Besides the contraceptive effect, the hormonal methods offer additional benefits. Several evidences support their use to prevent or to treat menstrual disorders such as irregular bleeding, menorrhagia and/or dysmenorrhea. Additionally, hormonal contraceptions are recommended for adolescent girls to decrease hyperandrogenism symptoms (acne and hirsutism) related to diagnosed Polycystic ovary syndrome (PCOS) or those considered to be at risk (39). Changes in hormone levels due to hormonal contraceptives can also significantly mitigate the symptoms in Premenstrual Syndrome (PMS) and Premenstrual Disphoric Disorder (PMDD). They can influence libido and vaginal health (39). Furthermore, hormonal contraceptives help to mitigate the migraine, reduce the risk of pelvic inflammatory disease, rheumatoid arthritis, asthma symptoms and preserve bone density. Finally, some hormonal contraceptives confer oncological prevention for ovarian, endometrial cancers and colorectal cancer (39, 40).
The choice of a contraceptive method
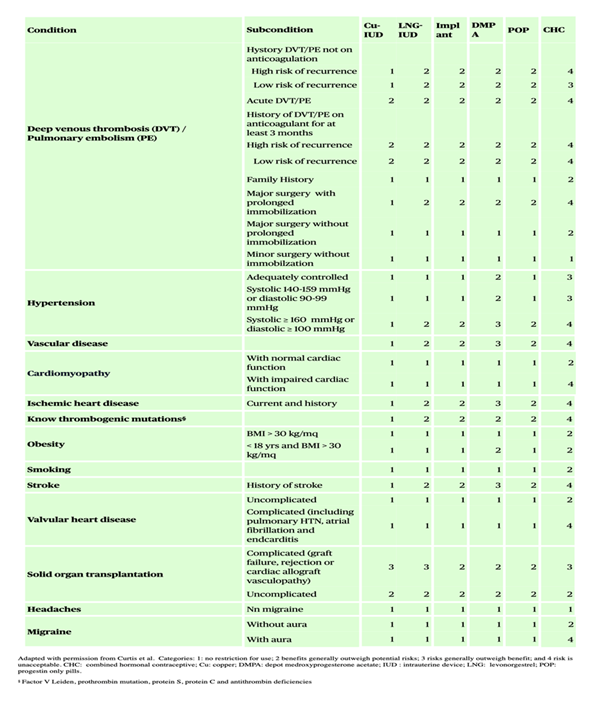
The choice of a contraceptive method is a complex decision. Medical Eligibility Criteria for Contraceptive Use (MEC) provides guidance on contraceptive options (41). The most appropriate method should be identify by a clinician-patient shared decision-making approach, evaluating the method efficacy, the safety profile, non contraceptive benefits, patient’s preference and compliance. There are not restrictions for adolescents to access the range of contraceptive options available to adults. However, generalized risks of the contraceptive methods should be considered in the setting of the individual specific cardiovascular condition (Fig.4). Special consideration should be given also to both acquired risk factors and/or sequelae from previous repairs or palliation that may influence the level of risk relating to the safety in using contraceptives.
Progestogen-only contraceptives are generally considered safe in the majority of women with CHDs, including adolescents and nulliparous. Because of their effectiveness and safety profile, they are recommended as first-line for high-risk women with CHDs. These options may be considered also in women who frequently experience user errors and women who anticipate experiencing user errors with user-dependent methods (e.g., oral contraceptive pills, the combined contraceptive transdermal patch, the combined contraceptive vaginal ring or barrier methods). The combined oral estro-progestinics contraceptive pills are generally not recommend in women at increased risk of thromboembolic events, for the susceptibility to thrombosis events and myocardial infarction (42,43). On the other hand, women with well-controlled hypertension may be eligible for a lower-dose hormonal option, although this decision should be made following a thorough assessment of their health and must involve regular monitoring to ensure that blood pressure remains within safe limits. In addition to non-barrier contraceptive methods (like oral contraceptives, IUDs, or implants), barrier method is strongly recommended in all patients as layer of protection against HIV and other STDs. This strategy should be used also in high-risk patient to bridge the efficacy gap if they are already using another effective method for pregnancy prevention (including women treated with Bosentan in which the endothelin receptor antagonist drug may reduce the efficacy of hormonal contraceptive methods) (1, 22).
During each medical consultation, it is essential to inquire about the patient’s correct use of contraception, assess for common side effects, and identify any signs or symptoms that warrant gynecological re-evaluation. In this setting, it is crucial to understand whether to continue or switch contraceptive methods according to unwanted side effects and patient’s preferences and priorities. Finally, appropriate health care services should be designed for patients requiring contraceptive methods that need surgical approaches for their insertion, fitting and/or removal(i.e. sterilization, implant, IUD, diaphragm, cervical cap) in order to reduce the risk of infection and/or complications. Similarly, the access to emergency contraceptions and/or voluntary termination of pregnancy termination should be offer to patients in safe and respectful health care setting with an experienced cardiac obstetric team. In this case, psychological support and appropriate counselling is recommended to prevent subsequent pregnancies in adolescents.
Termination of pregnancy in Teens
55% of unintended pregnancies among adolescent girls aged 15–19 years end in induced abortions (6). Termination of pregnancy should be proposed also in patients with CHDs for which the risk of maternal mortality or severe morbidity is unacceptably high. Medical regimes using Mifepristone and/or Misoprostol may be used in women with well-controlled cardiovascular diseases and stable conditions referred to outpatient procedure. Hospital based setting may be instead indicated for women undergoing either medical or surgical abortion in presence of conditions associated with highest risk of abortion-related cardiovascular events like as cyanotic diseases, pulmonary arterial hypertension, ventricular dysfunction, significant valvular disease and/or uncontrolled tachyarrhythmias. Additional post-operative inpatient monitoring should be considered for those patients, women who are at increased risk of post-operative complications, including those having a later second trimester termination or those receiving anticoagulant or anti-platelet agents (22, 44).
The importance of Counseling for healthy choices
More and more adolescents explore their sexuality precociously, but only few of them receive the preventive health counseling. Sexual and reproductive health issues include, but are not limited to puberty, reproduction aspects, contraceptions and STDs. They encompass in fact a wide range of learning about the cognitive, emotional, social, interactive and physical aspects of sexuality. The aim of a sexual counseling is to help raise informed, confident, and body-positive young people them to realize their health, well-being and dignity. Sex education should begin before the initiation of sexual activity and build over time. Parents are usually the first and most influential sex educators for teens. However, they use sometimes a conservative and overprotective approach providing inaccurate information which may lead to unnecessary fears and unhealthy risky behavior. Therefore, it is crucial that reproductive health informations would be systematically provide during medical appointments by a multidisciplinary cardio-obstetric team with experience in CHDs who can support and guide young patients in their sexual choices, finding a meeting point between their desires and their needs. Ideally, the sexual counseling should be provided in a timely fashion at around 12 to 13 years of age and continued throughout the entire transition from pediatric healthcare into adult age. The onset of menarche is the milestone for young women with CHDs to discuss about pregnancy and importance of planning or ways to prevent unwanted pregnancies.
A gynecologic history that includes menstrual patterns, sexual activity, and contraceptive use should be included in every clinic evaluation. Contents and strategies of communication should always be adequate to the patients’ psychological development. Confidentiality is a major factor contributing to adolescents feeling safe when discussing reproductive health with their health-care provider. The counseling should be tailored according to behaviors, values, and goals. The interaction with the adolescent should be carry out in an emphatic and nonjudgmental way. Usually, adolescents with more severe CHD are more likely to discuss relating to contraception and pregnancy. It may be related to more frequent clinic visits and/or recognizable fears for poor reproductive outcomes than those with other lesions (45). In addition, adolescents and young adults with moderate and complex CHDs lack adequate knowledge about life-long cardiac care and desire to learn more about the type of care that they will require in adulthood than patients with simplex diseases (46).
Finally, regardless of contraceptive choice, teens should be counseled about of the importance of condom use for preventing the transmission of STDs, including HIV. For women who are actively contemplating pregnancy, a rigorous risk stratification is necessary to assess the impact of a potential pregnancy on their cardiac condition, and viceversa, in order to optimize pre-pregnancy status and improve both maternal and neonatal outcome (10). Several models have been proposed to estimate the risk of foetal and maternal complications during and after pregnancy (1, 47, 48). When pregnancy is considered safe (mWHO I-II) , it is important to discuss the possibility of inheritance of the cardiac condition with the couple, as well as to clarify with the mother-to-be that associated comorbidities may change the prognosis of each patient with congenital heart disease in the same risk class during pregnancy (1, 48, 49).
Women for which the pregnancy is contraindicated (mWHO IV) or at high risk for pregnancy (mWHO III) (1,48, 49) should receive early counseling and a comprehensive discussion of their available options, including surrogacy, adoption and permanent forms of contraception (48, 49).
Conclusion
Adolescents with CHDs should be supported and guided by qualified professionals during the transition to adulthood. Reproductive and sexual health must not remain generational taboos but should instead become integral components of the comprehensive education of young adults, fostering self-awareness and informed decision-making. A tailored counseling is essential to prevent the STDs and unintended pregnancies, particularly in these populations at increased risk of complications. In this setting, the selection of an appropriate contraceptive method represents a critical decision-making process that must balance patient preferences, method safety, and contraceptive efficacy. Specific medical conditions and the potential for adverse effects related to particular contraceptive methods may pose significant limitations in method selection. Emergency contraception should be offered to individuals with CHD for whom the risk of maternal mortality is deemed unacceptably high.
References
- Baumgartner H, De Backer J, Babu-Narayan SV, et al. ESC Scientific Document Group. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J 42 (2021): 563-645.
- Marelli AJ, Mackie AS, Ionescu-Ittu R, et al. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation 115 (2007): 163-72.
- Gilboa SM, Devine OJ, Kucik JE, et al. Congenital Heart Defects in the United States: Estimating the Magnitude of the Affected Population in 2010. Circulation 134 (2016): 101-9.
- Haberer K, Silversides CK. Congenital Heart Disease and Women's Health Across the Life Span: Focus on Reproductive Issues. Can J Cardiol 35 (2019): 1652-1663.
- Burström Å, Acuña Mora M, Sparud-Lundin C, et al. Adolescents With Congenital Heart Disease: What Do They Know About Reproductive Health and Risks? J Cardiovasc Nurs 37 (2022): E172-E180.
- World Health Organization. Adolescent Pregnancy (2024).
- Vigl M, Kaemmerer M, Niggemeyer E, et al. Sexuality and reproductive health in women with congenital heart disease. Am J Cardiol 105 (2010): 538-41.
- Feyissa TR, Akter S, Harris ML. Contraceptive counselling and uptake of contraception among women with cardiovascular diseases: a systematic review and meta-analysis. Clin Res Cardiol 113 (2024): 1151-1170..
- Magnusson BM, Nield JA, Lapane KL. Age at first intercourse and subsequent sexual partnering among adult women in the United States, a cross-sectional study. BMC Public Health 15 (2015): 98.
- Loomba RS, Aggarwal S, Pelech AN. Addressing sexual health in congenital heart disease: when being the same isn't the same. Congenit Heart Dis 10 (2015): 30-5.
- Abma JC, Martinez GM. Teenagers in the United States: Sexual Activity,Contraceptive Use, and Childbearing, 2015-2019. Natl Health Stat Report 196 (2023): 1-23.
- Koerten MA, Szatmári A, Niwa K, et al. Evaluation of contraceptive methods in women with congenital heart disease in Germany, Hungary and Japan. Int J Cardiol 206 (2016): 13-8.
- Lindley KJ, Madden T, Cahill AG, et al. Contraceptive Use and Unintended Pregnancy in Women With Congenital Heart Disease. Obstet Gynecol 126 (2015): 363-369.
- Hinze A, Kutty S, Sayles H, et al. Reproductive and contraceptive counseling received by adult women with congenital heart disease: a risk-based analysis. Congenit Heart Dis 8 (2013): 20-31.
- Kasargod Prabhakar CR, Pamment D, Thompson PJ, et al. Pre-conceptual counselling in cardiology patients: still work to do and still missed opportunities. A comparison between 2015 and 2019 in women with cardiac disease attending combined obstetric cardiology clinics. Should the European Guidelines change anything? Cardiol Young 32 (2022): 64-70
- Miner PD, Canobbio MM, Pearson DD, et al. Contraceptive Practices of Women With Complex Congenital Heart Disease. Am J Cardiol 119 (2017): 911-915.
- Ott MA, Sucato GS; Committee on Adolescence. Contraception for adolescents. Pediatrics 134 (2014): e1257-81.
- Abarbanell G, Tepper NK, Farr SL. Safety of contraceptive use among women with congenital heart disease: A systematic review. Congenit Heart Dis 14 (2019): 331-340.
- Rabajoli F, Aruta E, Presbitero P, et al. Risks of contraception and pregnancy in patients with congenital cardiopathies. Retrospective study on 108 patients. G Ital Cardiol 22 (1992): 1133–1137.
- Pundi KN, Pundi K, Johnson JN, et al. Contraception Practices and Pregnancy Outcome in Patients after Fontan Operation. Congenit Heart Dis 11 (2016): 63-70.
- Trinh A, Vyas A, Roselle A, et al. Contraception and Cardiovascular Effects: What Should the Cardiologist Know? Curr Cardiol Rep 25 (2023): 1489-1498.
- Lindley KJ, Bairey Merz CN, Davis MB, et al. American College of Cardiology Cardiovascular Disease in Women Committee and the Cardio-Obstetrics Work Group. Contraception and Reproductive Planning for Women With Cardiovascular Disease: JACC Focus Seminar 5/5. J Am Coll Cardiol 77 (2021): 1823-1834.
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e35-e71. doi: 10.1161/CIR.0000000000000932. Epub 2020 Dec 17. Erratum in: Circulation. 2021 Feb 2;143(5):e228. doi: 10.1161/CIR.0000000000000960. Erratum in: Circulation 143 (2021): e784.
- Trussell J, Guthrie KA. Choosing a contraceptive: efficacy, safety, and personal considerations. In: Hatcher RA, Trussell J, Nelson AL, Cates W, Kowhal D, Policar M (eds). Contraceptive Technology: Twentieth Revised Edition. New York NY: Ardent Media (2011): 45-74.
- Milliren CE, DiVasta AD, Edwards AJ, et al. Contraceptive Implant-Associated Bleeding in Adolescent/Young Adult Clinical Practice: Associated Factors, Management, and Rates of Discontinuation. J. Adolesc Health 72 (2023): 583–590.
- Pitts S, Milliren CE, Borzutzky C, et al. Adolescent/Young Adult Long-Acting Reversible Contraception: Experience from a Multisite Adolescent Medicine Collaborative. J. Pediatr 243 (2022): 158–166.
- Wernick HJ, Abdel-Rasoul M, Berlan ED, et al. Body Mass Index Changes Among Adolescents and Young Adults Using the Etonogestrel Contraceptive Implant. Obstet Gynecol 144 (2024): 553-561.
- Oliveira JA, Neves GL, Pinhati MES, et al. Subdermal implants vs. levonorgestrel intrauterine devices outcomes in reproductive-aged women: a systematic review and meta-analysis. Arch Gynecol Obstet 311 (2025): 1173-1180.
- Patel J, Nguyen BT. Vasectomy: An Opportunity for Obstetricians and Gynecologists. Clin Obstet Gynecol 63 (2020): 289-294.
- Shih G, Zhang Y, Bukowski K, et al. Bringing men to the table: sterilization can be for him or for her. Clin Obstet Gynecol 57 (2014): 731-40.
- Famuyide AO, Hopkins MR, El-Nashar SA, et al. Hysteroscopic sterilization in women with severe cardiac disease: experience at a tertiary center. Mayo Clin Proc 83 (2008): 431-8.
- Teal S, Edelman A. Contraception Selection, Effectiveness, and Adverse Effects: A Review. JAMA 326 (2021): 2507-2518.
- Seth R, Moss AJ, McNitt S, et al. Long QT syndrome and pregnancy. J Am Coll Cardiol 49 (2007): 1092–1098.
- Grimes DA, Lopez LM, O'Brien PA, et al. Progestin-only pills for contraception. Cochrane Database Syst Rev (2013): CD007541.
- Roos-Hesselink JW, Cornette J, Sliwa K, et al. Contraception and cardiovascular disease. Eur Heart J 36 (2015): 1728-34.
- Vasilakis C, Jick SS, Jick H. The risk of venous thromboembolism in users of postcoital contraceptive pills. Contraception 59 (1999): 79-83.
- Jesam C, Cochon L, Salvatierra AM, et al. A prospective, open-label, multicenter study to assess the pharmacodynamics and safety of repeated use of 30 mg ulipristal acetate. Contraception 93 (2016): 310-316.
- Ellison J, Thomson AJ, Greer IA, Walker ID. Drug Points: Apparent interaction between warfarin and levonorgestrel used for emergency contraception. BMJ 321 (2000): 1382.
- Schindler AE. Non-contraceptive benefits of oral hormonal contraceptives. Int J Endocrinol Metab 11 (2013): 41-7.
- Bitzer J. Oral contraceptives in adolescent women. Best Pract Res Clin Endocrinol Metab 27 (2013): 77–89.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep 65 (2016): 1-103.
- Shufelt CL, Bairey Merz CN. Contraceptive hormone use and cardiovascular disease. J Am Coll Cardiol 53 (2009): 221-31.
- Lidegaard Ø, Løkkegaard E, Jensen A, et al. Thrombotic stroke and myocardial infarction with hormonal contraception. N Engl J Med 366 (2012): 2257-66.
- Guiahi M, Davis A; Society of Family Planning. First-trimester abortion in women with medical conditions: release date October 2012 SFP guideline #20122. Contraception 86 (2012): 622-30.
- Katz AJ, Lyon S, Farrell AG, et al. Adolescent Women with Congenital Heart Disease: Self-Reported Reproductive Health Discussions with Health Care Providers. J Pediatr Adolesc Gynecol 35 (2022): 299-304.
- Fernandes SM, Verstappen A, Clair M, et al. Adult Congenital Heart Association and the Adult Congenital Cardiac Care Associate Research Group. Knowledge of Life-Long Cardiac Care by Adolescents and Young Adults with Congenital Heart Disease. Pediatr Cardiol 40 (2019): 1439-1444
- De Backer J, Haugaa KH, Hasselberg NE, et al. ESC Scientific Document Group. 2025 ESC Guidelines for the management of cardiovascular disease and pregnancy. Eur Heart J (2025): ehaf193.
- Davis MB, Arendt K, Bello NA, et al. American College of Cardiology Cardiovascular Disease in Women Committee and the Cardio-Obstetrics Work Group. Team-Based Care of Women With Cardiovascular Disease From Pre-Conception Through Pregnancy and Postpartum: JACC Focus Seminar 1/5. J Am Coll Cardiol 77 (2021): 1763-1777.
- Wander G, van der Zande JA, Patel RR, et al. Pregnancy in women with congenital heart disease: a focus on management and preventing the risk of complications. Expert Rev Cardiovasc Ther 21 (2023): 587-599.