Creutzfeldt-Jakob Disease: A Case Report
Eda Harizi1, Kledisa Shemsi2, Ilir Ahmetgjekaj3, Tamanna Agarwal4, Elsie Tachie Mensah5, Alecya Anyim5, Blerina Saraci6, Denis Qirinxhi6, Grace Lin7, Fjolla Hyseni8, Mohamed Gamal9*, Sedjana Rrustemaj10*, Abdelrahman Awad11, Mohamed M Elgohary12, Mohamed Subahi13
1Department of Neurology, Regional Hospital of Durres, Albania
2Department of Psychiatry, Ginsburg Hospital, Germany
3Department of Radiology, Diagnostic Center, UCCK, Pristine City, Kosovo
4Faculty of Medicine in Hradec Kralove, Charles University in Prague
5Department of Internal Medicine, Mayo Clinic, Rochester, USA
6Department of Radiology, University of Medicine and UHC Mother Teresa, Tirana, Albania
7Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, USA
8Research scientist/Sonographer, NYU Langone Health, New York, USA
9Department of Radiology, Mayo Clinic, Rochester, USA
10Post -Baccalaureate Student, Cleveland State University, USA
11Department of Internal Medicine,Mansoura,Egypt
12Department of Neuro-Surgery, Mayo Clinic, Rochester, Minnesota, USA.
13Department of Cardiovascular Disease, Mayo Clinic Rochester Minnesota USA
*Corresponding Author: Mohamed Gamal, Department of Radiology, Mayo Clinic, Rochester, USA
Sedjana Rrustemaj, Post -Baccalaureate Student, Cleveland State University, USA
Received: 22 July 2025; Accepted: 28 July 2025; Published: 01 August 2025.
Article Information
Citation: Eda Harizi, Kledisa Shemsi, Ilir Ahmetgjekaj, Tamanna Agarwal, Elsie Tachie Mensah, Alecya Anyim, Blerina Saraci, Denis Qirinxhi, Grace Lin, Fjolla Hyseni, Mohamed Gamal, Sedjana Rrustemaj, Abdelrahman Awad, Mohamed M Elgohary, Mohamed Subahi. Creutzfeldt-Jakob Disease: A Case Report. Journal of Psychiatry and Psychiatric Disorders 9 (2025): 255-258.
DOI: 10.26502/jppd.2572-519X0256
Share at FacebookAbstract
Sporadic Creutzfeldt-Jakob Disease is a human spongiform encephalopathy caused by prions. It is a rapidly progressing neurodegenerative disease with death resulting within 12 months of disease onset. Clinically patients may present with a triad of progressive dementia, myoclonus and ataxia, accompanied by visual disturbances and psychiatric signs and symptoms. The patient presentation is largely non-specific and must be differentiated from other forms of dementia. This presents a challenge for physicians in diagnosing this rare condition. We present a 61- year-old woman with impaired consciousness and a rapidly worsening condition, with a suspected diagnosis of sporadic CJD.
Keywords
Sporadic Creutzfeldt-Jakob, Spongiform encephalopathy, Dementia, Prions.
Article Details
1. Introduction
Creutzfeldt-Jakob Disease (CJD) is an extremely rare, uniformly fatal neurodegenerative disease caused by prion proteins [1]. It is a progressive disease marked by rapid deterioration and ultimately death of the patient. It typically affects the elderly, with mean onset of the most common form, sporadic Creutzfeldt-Jakob disease (sCJD), to be 65 years [3]. Its annual incidence worldwide is 1-2 per million, making it challenging to diagnose as it is not readily suspected in patients. It belongs to the group of human spongiform encephalopathies, with prion proteins causing extensive neurological damage and degeneration. CJD is further characterized by rapidly progressive dementia, visual disturbances, myoclonus, psychiatric manifestations, cerebellar, pyramidal and extrapyramidal signs. The disease course leads to akinetic mutism and eventually death within 1 year of onset [1, 4]. The causative agent “prion” is named so due to its “proteinaceous” and “infectious” nature, referring to the previously unknown form of this infection due to protein misfolding in 1982 [1]. We present a 61-year-old woman with primarily psychiatric manifestations of CJD, without the classic triad typical of the disease.
2. Case Report
The patient was a 61-year-old woman who was admitted to the hospital due to impaired consciousness and a catatonic state. Prior to hospitalization, the patient’s health condition began gradually deteriorating, with fever, temperature, and impaired consciousness, followed by a catatonic state. The patient’s family also reported that she has recently had disagreements and problems at the workplace. She was initially hospitalized in the Department of Infectious Disease with the provisional diagnosis of Acute Psychotic Episode after which she was transferred to the Department of Psychiatry. A further worsening of her general health status necessitated a transfer to the intensive care unit. Her past medical history was non-contributory. She denied any hereditary conditions, suffered from arterial hypertension, and had taken two doses of the COVID-19 vaccine. Her physical examination was characteristic of her catatonic state, with irresponsiveness to external stimuli. Her upper and lower extremity reflexes and muscle strength could not be examined due to her catatonic condition. A series of lab and imaging tests were undertaken as part of the diagnostic work up. As measured with plasma, ALT GPT peak was 63U/L, 69U/L, and CRP peak was 180.7mg/L. From the images obtained through the magnetic resonance of the brain parenchyma, we inferred the possibility of a CJD diagnosis.
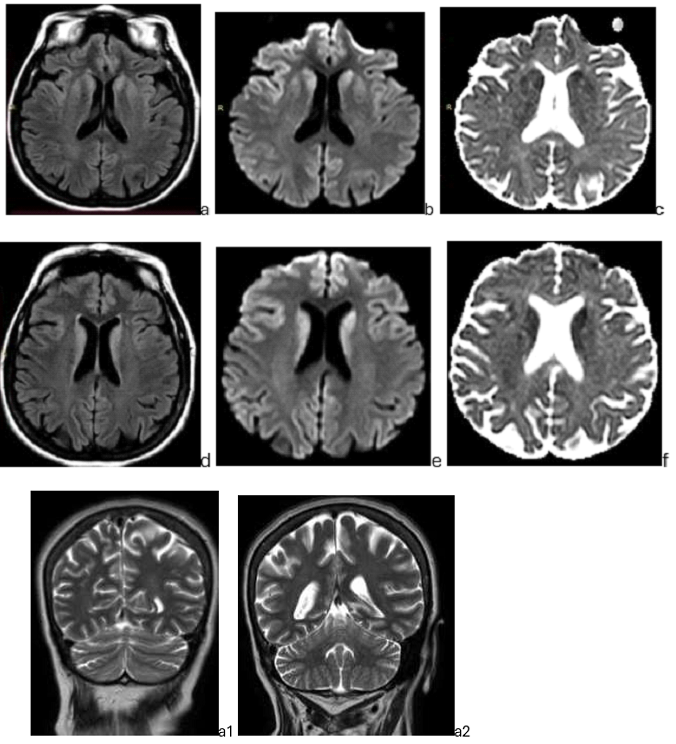
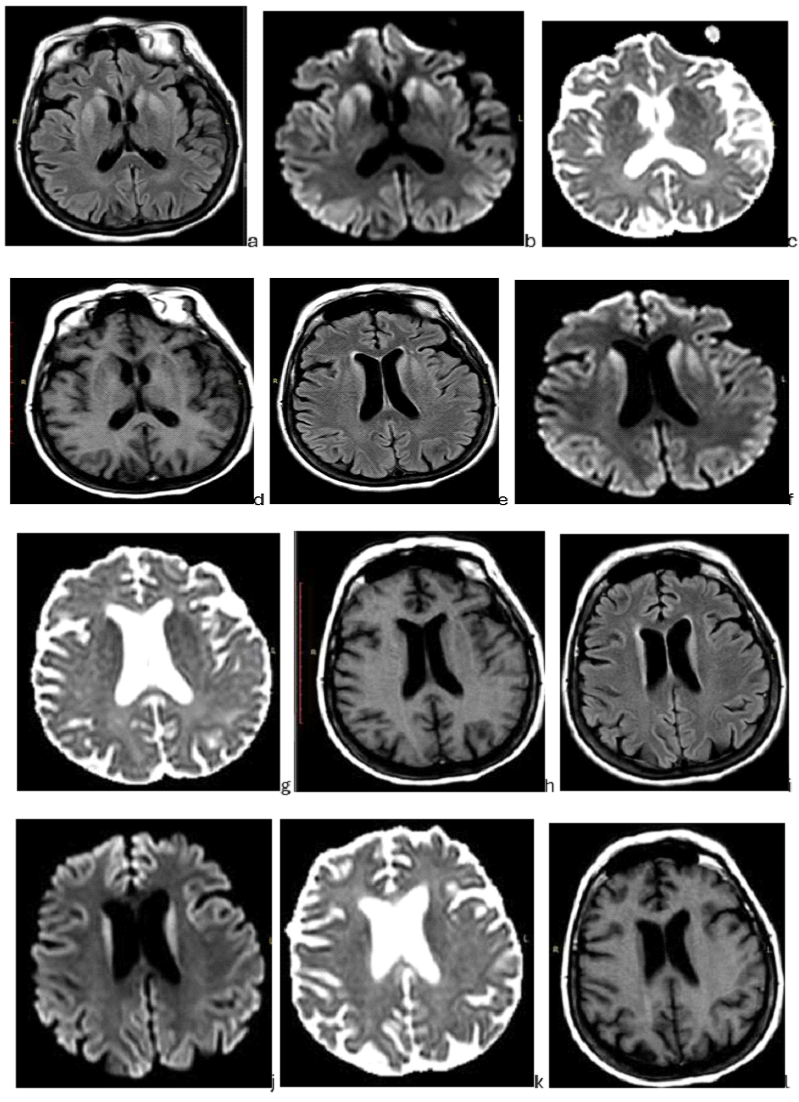
Hyperintense lesions in the FLAIR sequence with restricted water diffusion are symmetrically and bilaterally observed in the corpus striatum, respectively in the anterior putamen and nucleus caudatus, mainly the caput nuclei caudate. Aside from that, there are no other lesions restricting water diffusion. Circulation spaces at LCS remain unchanged. Large cerebral veins and dural sinuses have normal flow voids. A brain MRI after a one-month interval revealed no significant changes in the lesions. Prion encephalopathy was suspected to be the cause of these imaging changes. An electroencephalogram (EEG) was performed next that recorded periodic synchronous epileptiform discharge. Triphasic waves were present as well as generalized deceleration of electrocerebral activity. These EEG changes are typical for subacute spongiform encephalopathy, Creutzfeldt Jacob Disease. Additionally, the 14-3-3 protein found in the patient’s cerebrospinal fluid confirmed the diagnosis of CJD. Three months after being diagnosed with CJD the patient passed away.
Hyperintense signals in FLAIR and restriction of water diffusion are presented bilaterally and symmetrically in the corpus striatum, respectively in the anterior putamen and nucleus caudate, mainly the head of the caudate nucleus (caput nuclei caudate) bilaterally and symmetrically. LCS circulation spaces are unchanged. The lesions do not change much in time, almost not at all (about 1 month). There are no other diffusion-restricted lesions. Normal void flow in dural sinuses and great cerebral veins. Changes favor Creutzfeldt-Jakob disease.
3. Discussion
CJD is clinically heterogenous and though the triad of progressive dementia, myoclonus and ataxia is well known, other psychiatric and behavioral abnormalities may point to the disease. These signs are nonspecific, and the behavior and personality changes may obscure the accompanying characteristic cognitive decline. CJD dementia should be differentiated from other forms of dementia in the elderly such as Lewy body dementia or Alzheimer’s disease, which is also a disease of protein misfolding [2, 3, 4]. Sporadic CJD represents the commonest form of the disease in 85% of cases, occurring spontaneously. Genetic or familial CJD is the second most common form, representing 10-15% of cases and is caused due to autosomal dominant mutations in the gene encoding the prion protein. The rarest form of CJD is the iatrogenic or acquired which is transmitted from an infected human or animal and is less than 1% of cases. “Mad cow disease” or bovine spongiform encephalopathy is a variant form of CJD acquired by consuming beef infected by a bovine disease similar to human CJD [1, 2]. Normal cellular prion protein (PrP) is a normally occurring protein found on the membranes of cells in healthy humans and animals. The disease-causing form of prion PrP scrapie (PrPsc) is a normal PrP misfolded, this structurally changed prion behaves abnormally by self-propagating and accumulating throughout the brain [2]. This infectious form of the prion can also trigger normal PrP to convert to the infectious isoform. Together, the transformation of prion proteins into prions and the accumulation of misfolded, abnormal prions, is believed to lead to neurodegeneration [1]. The diagnosis is confirmed by pathological examination of brain tissue to detect the protease resistant PrPsc and is considered the gold standard. Non-invasive testing is considered sufficient to make a “probable” diagnosis of sporadic CJD [4]. MRI, EEG and CSF studies for protein 14-3-3 are primarily used to diagnose CJD, in failure of another diagnosis to be reached or in a high suspicion of CJD. EEG findings are characterized by periodic synchronous biphasic or triphasic sharp wave complexes in sporadic CJD. It is the least specific and is now less useful than the use of MRI and CSF testing. However, it remains an important part of the diagnostic process [2]. CSF protein 14-3-3 is a non-specific marker of neuronal death and is sensitive and specific to sporadic CJD with an accuracy of about 70%. Brain MRI with T2-weighted, diffusion-weighted imaging is far more accurate with a 97% diagnostic accuracy and reveals distinctive abnormalities in the brain associated with CJD [1]. Classically, bilateral, symmetrical hyperintensities are seen in the cerebral cortex, basal ganglia, and thalamus [6]. The variant form of CJD shows high signals in the pulvinar, termed the “hockey stick” or “pulvinar” sign. Rudge et al. showed that the brain MRI is the most useful test for screening patients with clinical suspicion of CJD and pointed out that an over-reliance on protein 14-3-3 may lead to an incorrect diagnosis of CJD. The introduction of the new real-time quaking-induced conversion (RT-QuIC) to detect small amounts of PrPsc is considered more promising and secure in delivering a diagnosis of CJD compared to protein 14-3-3. RT-QuIC monitors the formation of misfolded PrP in real time using fluorescence via fluorescent dye thioflavin. A CSF sample from the patient is added to recombinant PrP and thioflavin. The PrPsc binds to and induces misfolding of the recombinant PrP, much like in the brain tissue of humans [8]. RT-QuIC has high sensitivity in diagnosing CJD with studies reporting between 82-96% [2, 7]. Currently, no curative treatment exists for sporadic CJD and efforts are directed towards palliative care and emotional support for the patient and family. Opioid based pain relief and sodium valproate and clonazepam are recommended for treating the myoclonus [4, 5]. Drug trials on CJD have been carried out but without success.
Conclusion
As demonstrated by our patient, sporadic CJD patients may present with psychiatric problems masking the underlying neurological degeneration. This requires vigilance and sufficient knowledge of the disease by physicians.
Early and accurate diagnosis of sporadic CJD, differential from other dementias or possible treatable infectious causes of encephalitis is crucial in preparing the family for the disease course of sporadic CJD.
References
- Sitammagari KK, Masood W. Creutzfeldt Jakob Disease. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2022).
- Mackenzie G, and Will R. Creutzfeldt-Jakob disease: recent developments. F1000Research 6 (2017): 2053.
- Kojima G, Tatsuno B K, Inaba M, et al. Creutzfeldt-Jakob disease: a case report and differential diagnoses. Hawai'i journal of medicine & public health: a journal of Asia Pacific Medicine & Public Health 72 (2013): 136-139.
- Raut A, Thapa A, Shrestha A, et al. Creutzfeldt-Jakob disease: A case report and differential diagnoses. Clinical case reports 10 (2022): 6239.
- Ojha R, Nepal G, Jamarkattel S, et al. Sporadic Creutzfeldt-Jakob disease: A case report and review of literature. Clinical case reports 8 (2020): 2240-2244.
- Schröter A, Zerr I, Henkel K, et al. Magnetic Resonance Imaging in the Clinical Diagnosis of Creutzfeldt-Jakob Disease. Arch Neurol 57 (2000): 1751-1757.
- Rudge P, Hyare H, Green A, et al. Imaging and CSF analyses effectively distinguish CJD from its mimics Journal of Neurology, Neurosurgery & Psychiatry 89 (2018): 461-466.
- Green A. RT-QuIC: a new test for sporadic CJD. Practical neurology 19 (2019): 49-55.