Efficacy of Tramadol Hydrochloride with added Adrenaline and Tramadol Hydrochloride without Adrenaline as local anesthetic
Gourab Paul*, Hiralal Ash, Anu Singh, Abhishek Kumar, Swastika Sen
Department of Oral & Maxillofacial surgery, Buddha Institute of Dental Sciences and Hospital, West of TV Tower, Gandhinagar, Kanti Factory Rd, Kankarbagh, Patna, Bihar 800020, India
*Corresponding Author: Dr. Gourab Paul, Department of Oral & Maxillofacial surgery, Buddha Institute of Dental Sciences and Hospital, West of TV Tower, Gandhinagar, Kanti Factory Rd, Kankarbagh, Patna, Bihar 800020, India.
Received: 28 June 2025; Accepted: 07 July 2025; Published: 29 July 2025
Article Information
Citation: Gourab Paul, Hiralal Ash, Anu Singh, Abhishek Kumar, Swastika Sen. Efficacy of Tramadol Hydrochloride with added Adrenaline and Tramadol Hydrochloride without Adrenaline as local anesthetic. Journal of Surgery and Research. 8 (2025): 365-371.
Share at FacebookAbstract
Introduction: Local anesthetics are agents that reversibly interfere with neural conduction and are widely used to provide pain control in dental treatments. Tramadol has been reported to have anesthetic activity on peripheral nerves. When administered locally, it has both analgesic and anesthetic properties. The purpose of our study was to compare the local anesthetic effect of tramadol hydrochloride solution with adrenaline versus tramadol hydrochloride solution without adrenaline for nonsurgical extraction of maxillary tooth.
Materials and Methods: This double blinded randomized study was conducted in the department of oral & maxillofacial surgery of Buddha Institute of Dental Sciences and Hospital, Patna. A total 100 patients were selected from study population and randomly divided by lottery method in two groups who required extraction of maxillary tooth by intra alveolar method. GROUP A (50 patients)- Each patient received an initial dose of 1 syringe (1.8 mL) of drug A (mixture of tramadol HCl 50 mg and adrenalin 0.0225 mg diluted to 1.8 mL by distilled water). GROUP B (50 patients)- Each patient received an initial dose of 1 syringe (1.8 mL) of drug B (tramadol HCl 50 mg diluted to 1.8 mL by distilled water).
Results: We observed significant difference in Pain, Number of used syringe and per-operative bleeding whereas non-significant difference in Onset between group A and group B (p=0.092).
Conclusion: Supraperiosteal infiltration of tramadol HCl in combination with adrenaline was shown to be a very effective local anesthetic for the extraction of upper teeth and can be used as an alternative local anesthesia.
Keywords
Extraction, Maxillary tooth, Tramadol HCl, Adrenaline
Extraction articles; Maxillary tooth articles; Tramadol HCl articles; Adrenaline articles
Article Details
Introduction
Pain, as defined by the International Association for the Study of Pain, is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.” The Institute of Medicine Committee on Pain, Disability, and Chronic Illness Behavior highlighted the complex nature of pain by noting that experience of pain is more than a simple sensory process; it is a complex perception involving higher levels of the central nervous system, emotional states, and higher mental processes [1].
Oral pain is associated with pulpitis, pericoronitis, abscess (endodontic/periodontal), trauma, and other conditions including temporomandibular disorders (TMDs) and masticatory muscle disorders. Pain is provoked when a variety of inflammatory mediators such as bradykinin, histamine, leukotrienes, and prostaglandin E2 are released into the tissues. These pain-inducing substances can be produced and released from cell membranes by trauma (eg, mechanical trauma to the soft tissues and bone during periodontal surgery), infection, and allergenic reactions. There-fore, part of the successful management of pain requires managing the development of inflammation [2].
In dentistry, local anesthetics, which temporarily block nerve conduction without affecting patient consciousness, are widely used. The selection of the local anesthetic material to be used is very important in order to keep the anxiety level of the patients at a minimum and to make the treatments more painless and comfortable for the patients [3].
Local anesthetics are agents that reversibly interfere with neural conduction and are widely used to provide pain control in dental treatments, especially tooth extraction. Cocaine was the first drug used as a local anesthetic agent. However, because of its serious side effects, researchers searched for safer drugs. In the previous century, many safe local anesthetics were introduced, such as lidocaine in 1948, mepivacaine in 1957, prilocaine in 1960, and bupivacaine in 1963. Of these anesthetic agents, lidocaine hydrochloride (lidocaine HCl) is one of the most widely used agents in dentistry. Lidocaine HCl provides fast relief, has excellent anesthetic effects, and has minimal allergenicity [4].
Recently, in vitro and in vivo studies have shown that opioids such as diamorphine, meperidine and fentanyl have also local anesthetic effects besides their analgesic properties. One of these opioids is tramadol hydrochloride which is a well-known centrally acting opioid analgesic. Clinically, it has been used for many years in the treatment of moderate to severe pain and produces analgesia against multiple pain types such as postsurgical, obstetric, terminal cancer and neuropathic pain. Tramadol exerts a double action, functioning as both an opioid and a non-opioid although classified as a weak opioid in terms of analgesic properties. In nonopioid analgesic mechanism, it acts on inhibition of the reuptake of monoaminergic receptors such as norepinephrine and serotonin that are released from nerve endings. In this way it inhibits the transmission of pain in the central nervous system and blocks nociceptive impulses. So, this property creates a combined analgesic/adjuvant effect.
In contrast, tramadol has been reported to have anesthetic activity on peripheral nerves. It produces peripheral anti nociceptive effects by interaction with peripheral opioid receptors. When administered locally, it has both analgesic and anesthetic properties. In the literature, intradermal application of tramadol was shown to have a local anesthetic effect and when used with mepivacaine, it also prolongs brachial plexus blockade. It was also stated that tramadol can be used as a local anesthetic for the excision of small cutaneous lesions. Some authors state that tramadol possesses anaesthetic properties similar to lidocaine or prilocaine. In addition to the analgesic activity, its anesthetic efficacy has also been shown as an additive effect in inferior alveolar nerve block when used in combination with articaine. Similarly in another study, submucous local administration of tramadol was shown to increase the anesthetic efficacy of mepivacaine with epinephrine in inferior alveolar nerve blockade [3].
Tramadol is an atypical opioid, a racemic mixture of two isomers that was introduced as a centrally acting analgesic but has recently also been suggested to provide a local anesthetic effect similar to that of lidocaine and prilocaine. Tramadol exerts its analgesic action by activating both opioid and nonopioid mechanisms. Tramadol possesses opioid agonist properties selective for mu receptors as well as a nonopioid alpha2 agonistic and serotonergic pain inhibitory effect, acting as a 5-hydroxytryptamine and norepinephrine inhibitor for nerve endings. T" Pang and colleagues identified the local anesthetic properties of tramadol, metoclopramide, and lidocaine following intradermal injection and compared the peripheral analgesic effect of tramadol in reducing propofol injection pain with lidocaine. Altunkaya and colleagues demonstrated that intradermal tramadol provides local anesthesia similar to prilocaine in minor surgical procedures, whereas Kargi and colleagues were the first to conduct a pilot study for local infiltrative anesthesia comparing tramadol plus adrenaline to lidocaine plus adrenaline in hand surgery.
However, the local anesthetic effect of tramadol HCl in oral and maxillofacial surgery has not been studied vividly. The purpose of our study was to compare the local anesthetic effect of tramadol hydrochloride solution with adrenaline versus tramadol hydrochloride solution without adrenaline for nonsurgical extraction of maxillary tooth.
Materials and Methods
This double blinded randomized study was conducted in the department of oral & maxillofacial surgery of Buddha Institute of Dental Sciences and Hospital, Patna. The study was approved by the local academic committee according to relevant guidelines. Informed consent was obtained prior to inclusion in the study. Patients of both genders in the age group of 18-65years who required extraction of maxillary tooth were included in the study. Patient with history of systemic disease, Allergy or contraindication to drugs or anesthesia used in the study, pregnancy or lactation, Any noticeable local inflammation or pathology and Impacted tooth are excluded from the study.
A total 100 patients were selected from study population and randomly divided by lottery method in two groups who required extraction of maxillary tooth by intra alveolar method.
GROUP A (50 patients)- Each patient received an initial dose of 1 syringe (1.8 mL) of drug A (mixture of tramadol HCl 50 mg and adrenalin 0.0225 mg diluted to 1.8 mL by distilled water).
GROUP B (50 patients)- Each patient received an initial dose of 1 syringe (1.8 mL) of drug B (tramadol HCl 50 mg diluted to 1.8 mL by distilled water).
The same investigator performed all surgical procedures without having any idea about the type of drug used. The patient preoperative, intraoperative and postoperative treatment findings were recorded in a performa which was later subjected to statistical analysis.
Procedure
The study drugs for the 2 groups were prepared by an independent investigator in the Department, who was not involved in the surgical procedure. Syringes of drugs A and B had a similar appearance and were coded and blinded to the investigator and the participants.
Both solutions (Figure 1) were similar in appearance and a standard dental aspirating syringe fitted with a 27-gauge, 1.5-inch needle was used for injections. Buccal infiltrative anesthesia was performed under sterile conditions and in addition to a few drops of palatal injection by the same surgeon. Each patient received an initial dose of 1 dental syringe (1.8 ml) of drug.
The same investigator performed all surgical procedures without having any idea about the type of drug to be used.
In each case gingival separation was performed 3 minutes after administration of the local anesthetic solution. A closed extraction was carried out. The patient was instructed to inform the investigator about the degree of pain at any time during extraction by moving or raising the left hand. The degree of pain was evaluated with a 10-cm visual analog scale (VAS). Before starting treatment, the investigator explained the VAS to the patient. The VAS consisted of an interval scale ranging from 0 (no pain or discomfort) to 10 (maximum pain). During the extraction, when the VAS exceeded 3 points, an additional (0.9 mL) of the same drug was injected into the extraction site.
Following both infiltration anesthesia, the following measurements were made
Pain assesment
The degree of per operative pain was evaluated with VAS scale. The VAS consisted of an interval scale ranging from 0 (no pain or discomfort) to 10 (maximum pain).
Volume of anesthetic solution used
During the procedure total volume of anesthetic was noted by the number of syringes used, where each syringe contend 1.8ml of solution
Assessment of side effects
Local side effects, per operative and postoperative (immediate) such as erythema, swelling, irritation were recorded along with systemic side effects both per operative and postoperative (24hrs) like nausea, vomiting. Nausea and vomiting are common adverse effects of tramadol HCl. Persistent nausea (defined as an urge to vomit lasting >30 minutes) and at least 2 episodes of vomiting were treated with an intravenous injection of metoclopramide 10 mg. Nausea and vomiting were recorded using a 3-point ordinal scale (0, none; 1, nausea; 2, vomiting). Patients were reviewed after 24 hours and information about adverse effects was recorded.
Vital signs
Preoperative, per operative and postoperative (immediate) vital signs such as Blood Pressure recorded with sphygmomanometer, Pulse Rate and Peripheral Oxygen Saturation recorded with pulse oxymeter, Respiration Rate were recorded.
Bleeding
Per operative bleeding according to Likert scale was measured. Per operative bleeding assessment by the operator were presented with 1 anchored by “a few bleeding” and 5 anchored by “very much bleeding [5].”
Statistical analysis and observations
Statistical analysis
The data were entered in the excel sheet and were presented as percentage or Mean±SD. Mann Whitney test (nonparametric test) was applied to compare the difference between two unpaired groups using statistical analysis software SPSS (version 16). P value ≤0.05 was considered as significant.
Both the group were comprised of female (24%, 48%) and male (26%, 52%) and the mean age of group A was 43.32±14.35 and group B was 44.48±12.95.
Table 1, we observed non-significant difference in BP between both group at Pre-operative, Per-operative and Post-operative. At pre-operative the BP of group A was 122.88/74.40 and group B was 122.48/75.12, at per-operative it was 12.84/73.80 in group A and 122.48/75.12 in group B and at post-operative in group A it was 122.96/72.68 and 123.28/74.64 in group B.
|
BP |
Group A |
Group B |
P value |
|||
|
Mean |
SD |
Mean |
SD |
|||
|
Pre-operative |
Sys |
122.88 |
8.63 |
122.48 |
9.26 |
0.8 |
|
Dys |
74.4 |
7.8 |
75.12 |
7.76 |
0.537 |
|
|
Per-operative |
Sys |
123.84 |
8.05 |
122.48 |
9.26 |
0.463 |
|
Dys |
73.8 |
7.05 |
75.12 |
7.76 |
0.264 |
|
|
Postoperative |
Sys |
122.96 |
7.68 |
123.28 |
9.1 |
0.994 |
|
Dys |
72.68 |
6.1 |
74.64 |
6.42 |
0.101 |
|
Table 1: Comparison of Blood Pressure between Group A and Group B at Pre-operative, Per-operative and Postoperative.
We observed non-significant difference in PR between both group at Pre-operative, Per-operative and Post-operative. At pre-operative the PR of group A was 75.80±5.58 and group B was 74.88±5.40 (p=0.372), at per-operative it was 76.94±5.66 in group A and 76.16±6.07 in group B (p=0.296), and at post-operative in group A it was 76.80±5.55 and 76.62±6.51 in group B (p=0.545).
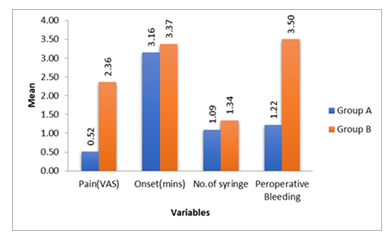
In table 2, we observed significant difference in Pain, Number of used syringe and per-operative bleeding whereas non-significant difference in Onset between group A and group B (p=0.092). The Pain in group A was 0.52±0.71 and group B was 2.36±1.71 (p=0.0001), Onset value was 3.16±0.66 in group A and 3.37±0.65 in group B (p=0.092), number of used syringe in group A was 1.09±0.26 and 1.34±0.31 in group B (p=0.0001) and per-operative bleeding was 1.22±0.46 in group A and 3.50±0.99 in group B (0.0001) (Figure 2).
|
Variables |
Group A |
Group B |
P value |
||
|
Mean |
SD |
Mean |
SD |
||
|
Pain (VAS) |
0.52 |
0.71 |
2.36 |
1.71 |
0.0001 (s) |
|
Onset (mins) |
3.16 |
0.66 |
3.37 |
0.65 |
0.092 |
|
No.of syringe |
1.09 |
0.26 |
1.34 |
0.31 |
0.0001 (s) |
|
Peroperative Bleeding |
1.22 |
0.46 |
3.5 |
0.99 |
0.0001 (s) |
Table 2: Comparison of Pain(VAS), Onset(mins), Volume of anesthetic solution used(Number of syringe) and Peroperative Bleeding between Group A and Group B.
Figure 2: Comparison of Pain(VAS), Onset(mins), Volume of anesthetic solution used(Number of syringe) and Peroperative Bleeding between Group A and Group B.
We observe no erythema and swelling at per and post-operative stage in group A and group B. We observed non-significant difference systematic side effect between group A and group B at in per and post-operative. At per-operative systemic side effect in group A was 0.06±0.24 and group B was 0.02±0.14 (p=0.31) and at post-operative it was 0.08±0.40 in group A and 0.02±0.14 in group B (p=0.544).
Discussion
Pain is the most commonly reported symptom by patients during dental extraction. Therefore, performing pain-free procedures is vital for healthcare professionals. Many studies have been performed on pain-free procedures. One way to achieve a pain-free procedure is to use local anesthesia. Local anesthesia is a molecule with an amide or ester group. However, the most commonly used local anesthetic agent is lignocaine, which is an amide [4].
The general incidence of complications related to local anaesthesia has been reported to be 4.5% (Daublander et al., 1997), whereas others have reported a prevalence of up to 26% (Kaufman et al. 2000). However, most reactions are likely low risk and transient. These adverse reactions can be classified into drug toxicity, drug allergy, local anaesthetic adjunct allergy, vasoconstrictor adjunct response and drug-specific responses (e.g. methemoglobinemia) (Finder and Moore, 2002) [6].
Hence, there is a need to ascertain a drug that provides an alternative to conventional local anaesthetics for individuals allergic to esters and amide. Opioids have been successfully used for pain management for many decades. Some of the opioids are known to have local anaesthetic action also [7].
Tramadol HCl may have local anesthesia-like activity because of its nerve conduction blocking potency. This is comparable to that of the local anesthetic agent lidocaine. The nerve conduction blocking effects of opioids have been shown to be fully reversible. (mother) In recent experimental and clinical studies by Al-Haideri YA, Kapral S et al. and Kakagia D et al. the peripheral local anaesthetic effect of tramadol was elucidated. Injection of 5% tramadol in soft tissue lesions via intradermal route proved to have a local anaesthetic effect similar to 2% lidocaine. The effect of tramadol anaesthesia has also been investigated in dentistry where Jaber L et al. demonstrated the presence of muopioid receptors in human coronal and radicular pulp tissue of human teeth, which indicates that peripheral anaesthetic effects of opioid agonists are induced by interaction with peripheral opioid receptors [7].
Danic P et al. the mechanism of local anaesthesia of tramadol as follows. Weak peripheral agonism over peripheral mu-opioid receptors whose number is heightened in hyperalgesia and inflammatory conditions, favouring the opening of nonspecific voltage-dependent potassium channels, acting in the nitric oxide pathway, agonistic action on vanilloid receptor one that apart from local analgesic effect, exerting undesired local side effects, such as burning pain and erythema, with a high concentration of tramadol blockade of the N-methylD-aspartate receptors and direct blocking of voltage-dependent sodium channels explains the local anaesthetic effect of tramadol [6].
Our study was to compare the local anaesthetic effect associated various parameters such as pain assessment, volume of anesthetic solution used, vital signs, per-operative bleeding of tramadol hydrochloride solution with adrenaline versus tramadol hydrochloride solution without adrenaline in extraction of maxillary tooth.
Both the group in the study comprised of female 24 (48%) and male 26 (52%) and the mean age of group A was 43.32±14.35 and group B was 44.48±12.95.
At pre-operative the mean Blood pressure of group A was 122.88/74.40 and group B was 122.48/75.12, at per-operative it was 12.84/73.80 in group A and 122.48/75.12 in group B and at post-operative in group A it was 122.96/72.68 and 123.28/74.64 in group B. We observed non-significant difference in blood pressure. Similarly Srivastava M et al. compared the local anesthetic efficacy of tramadol hydrochloride (with adrenaline) versus lignocaine hydrochloride (with adrenaline) in non-surgical tooth extractions reported that systolic and diastolic blood pressures were within the physiologic limits throughout the non-surgical extraction procedure in both the groups.
The Mean Respiratory rate at pre-operative of group A was 18.38±2.50 and group B was 17.76±2.37 (p=0.351), at per-operative it was 19.20±2.91 in group A and 18.38±2.66 in group B (p=0.166), and at post-operative in group A it was 18.38±2.50 and 17.76±2.78 in group B (p=0.351). There was non-significant difference in respiratory rate. Regmi NK et al. designed a study to compare the analgesic efficacy of tramadol used as an adjuvant to bupivacaine for supraclavicular brachial plexus block in patients undergoing orthopaedic surgeries of upper limb. The study suggests that tramadol when added to bupivacaine 2 for supraclavicular brachial plexus block enhances the quality of anaesthesia and analgesia without affecting respiratory rate.
At pre-operative the mean Pulse Rate of group A was 75.80±5.58 and group B was 74.88±5.40 (p=0.372), at per-operative it was 76.94±5.66 in group A and 76.16±6.07 in group B (p=0.296), and at post-operative in group A it was 76.80±5.55 and 76.62±6.51 in group B (p=0.545). We observed non-significant difference in Pulse rate between both group at Pre-operative, Per-operative and Post-operative. Similarly Regmi NK et al. in the above mentioned study found out that the pulse rate was within the normal range.
The saturation pre-operative of group A was 99.76±0.56 and group B was 99.78±0.91 (p=0.267), at per-operative it was 99.76±0.56 in group A and 99.78±0.91 in group B (p=0.267), and at post-operative in group A it was 99.84±0.42 and 99.82±0.75 in group B (p=0.553). Similarly peripheral capillary oxygen saturation was non-significant at Pre-operative, Per-operative and Post-operative. Similarly Regmi NK et al. in his study with tramadol mentioned stability of peripheral capillary oxygen saturation throughout.
In our study we observed no local complications like erythema and swelling at per-operative and post-operative stage in group A and group B. Likewise M.B. Passavanti et al. studied the efficacy of tramadol as local anaesthetic in reconstructive plastic surgery and reported no significant differences in incidence of local reactions like local site inflammation in both groups and no patient referred pain during the infiltration of drugs. Also Kargi E et al. in his study with tramadol as a local anaesthetic in tendon repair surgery of the hand mentioned about no significant skin reaction similar to our study [8,9]. At per-operative systemic side effect (nausea/vomiting) in group A was 0.06±0.24 and group B was 0.02±0.14 (p=0.31) and at post-operative it was 0.08±0.40 in group A and 0.02±0.14 in group B (p=0.544). We also observed non-significant difference in systematic side effect like nausea and vomiting between group A and group B at in per and post-operative. In a study conducted by Alsandook et al. tramadol (with adrenaline) induced nausea in 6.45% and vomiting in 1.61% of patients while lignocaine (with adrenaline) induced nausea in 2.23% of patients with no incidence of vomiting and there was no statistical significant difference between the two groups.Al-Haideri stated that of the 50 patients in the group using tramadol and adrenaline combination only 1 had nausea and vomiting, while in the group using pure tramadol, these side effects were seen in 3 patients. Similarly, Ege et al. reported that in the epinephrine-free tramadol group, 3 patients had dizziness and 1 patient had nausea among a group of 50 patients; whereas, in the lidocaine group only 1 patient had dizziness. All of these studies showed that there is no significant difference with respect to the side effects [10,11].
Shoeb Kasim Jendi and Abhishek Talathi studied to evaluate and compare the soft tissue anaesthesia produced by tramadol hydrochloride on gingival tissues in maxilla, mentioned that all participants tolerated well for intraoral procedures. Per operative bleeding according to Likert scale was measured. Per operative bleeding assessment by the operator were presented with 1 anchored by “a few bleeding” and 5 anchored by “very much bleeding [12,13].”
Less per-operative bleeding is observed in Group A is because of predominant α receptor stimulation, and hemostasis due to the presence of vasoconstrictor. Mean Per-operative bleeding was 1.22±0.46 in group A and 3.50±0.99 in group B (p=0.0001), showing significant difference. Studies by Stanley F Malamed mentioned that adding vasoconstrictors to local anaesthetic agents decreases surgical site bleeding on using vasoconstrictors as adjunct to local anaesthesia showing similar results like our study where and per-operative bleeding is minimal in Group A.
The volume of anesthetic solution used in Group A was less compared to Group B is due to presence of adrenaline. As adrenaline is a vasoconstrictor it causes constrictions of the surgical site capillaries thereby slowing the absorption rate of the local anesthetic solution.
In our study significant difference was also present in the number of used syringe. Average number of which in group A was 1.09±0.26 and 1.34±0.31 in group B (p=0.0001). This finding denotes the volume of anaesthetic solution used in both the groups. A study conducted by Al-Haideri where he divided two groups one with tramadol plus adrenaline another with plain tramadol and reported similar finding like our study where the volume of anesthetic solution required was less in adrenaline group [14].
The mean VAS score for group A (tramadol HCL with adrenaline) was comparatively less than group B (tramadol). In our study we observed significant difference in pain. The mean pain in group A was 0.52±0.71 and group B was 2.36±1.71 (p=0.0001). Studies by Stanley F Malamed mentioned that adding vasoconstrictors to local anaesthetic agents increases the depth of anaesthesia, similar to our study where mean VAS score was less in Group A compared to Group B.
Al-Haideri in a study where comparison of local anesthetic efficacy of tramadol hydrochloride (with adrenaline) versus plain tramadol hydrochloride in the extraction of upper molar teeth was done mentioned that per-operative VAS score was significantly low in vasoconstrictor group showing result like our study [14].
Basu S et al. in a study evaluated the efficacy of tramadol as a local anesthetic effect with respect to lignocaine and published that tramadol has an almost similar local anesthetic efficacy with that of lignocaine [15].
Madhuri S. Kurdi conducted a study to evaluate the effect of tramadol as a local anaesthetic and postoperative analgesic when compared with lignocaine for minor surgeries. Participants were randomly assigned to receive either 2mg/kg of tramadol with 1:2,00,000 adrenaline or 1mg/kg of lignocaine with 1:2,00,000 adrenaline. Similar to our study it was concluded that tramadol with adrenaline is a good local anaesthetic cum postoperative analgesic for minor surgical procedures [16].
Srivastava M et al. allocated patients randomly into 2 groups. Group T, each patient received (5% Tramadol HCl and adrenaline 1:80000); & Group L (2% Lidocaine HCL with adrenaline 1: 80000). He suggested that Tramadol HCL can be used as alternative to Lidocaine HCL in combination with adrenaline to achieve local anesthesia in situation where Lidocaine HCL is contraindicated [17].
Manu Goel et al. compared the effectiveness of tramadol to lignocaine as local anaesthesia in the extraction of firm teeth and found out that it should be used as a supplement to lignocaine in extensive surgical procedures [18].
Similarly Bilal Ege et al. compared the anesthetic efficiency of lidocaine and tramadol hydrochloride in orthodontic extractions and mentioned that tramadol hydrochloride can be a good alternative to local anesthetic agents and beneficial to support anesthesia during long operations [19].
U Siva Kalyan reported buccal infiltration of tramadol hydrochloride was an effective local anaesthesia for extraction of anterior maxillary teeth [20].
In our study, there was a significant difference between groups A and B in the volume of local anesthetic solution administered to produce local anesthesia, in levels of intraoperative pain and in the amount of per-operative bleeding. Thus Group A produced perfect local anesthesia and allowed painless extraction of upper teeth with comparatively minimal bleeding. This difference may be due to the presence of adrenaline in combination with tramadol HCl (group A), which produces vasoconstriction and confines the tramadol HCl locally to produce its effects on the nerve perfectly.
Conclusion
We see that tramadol HCl with adrenaline exhibits a local anesthetic effect that enables the surgeon to perform painless extraction of upper teeth when it is infiltrated and injected to susceptible neurons by a supraperiosteal infiltration technique. In contrast, supraperiosteal infiltration of tramadol HCl provides weak local anesthesia (in relation to the large volume).
Thus from our study we can say that supraperiosteal infiltration of tramadol HCl in the upper region produced weak local anesthesia for tooth extraction. Supraperiosteal infiltration of tramadol HCl in combination with adrenaline was shown to be a very effective local anesthetic for the extraction of upper teeth and can be used as an alternative local anesthesia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Merskey H, Bogduk N. Classification of chronic pain (ed 2). Seattle, WA, IASP, 1994
- Anxiety and pain management in dental office R. Kalai Selvi Ravishankar Undergraduate Saveetha institute of medical and technical sciences 162, Poonamallee High Road Chennai-600095, India.
- Osterwels M, Kleinman A, Mechanic D. Pain and disability. Washington, DC, National Academy press (1987).
- Milgrom P, Coldwell SE, Getz T, et al. Four dimensions of Fear of dental injections. Journal of the American Dental Association 128 (1997):756.
- Myong-H, Fiona DP, Moonkyu K et al. Comparison of the efficacy and safety of 2% lidocaine HCl with different epinephrine concentration for local anesthesia in participants undergoing surgical extraction of impacted mandibular third molars. Medicine 96 (2017): 21
- Malamed SF. Local anesthetic considerations in dental specialties. In: Handbook of Local Anesthesia. (5th edtn), (2004): 274.
- Bilal E, Miray E, Mahmut K, Hilal A. Comparison of the Anesthetic Efficiency of Lidocaine and Tramadol Hydrochloride in Orthodontic Extractions: A Split-Mouth, Prospective, Randomized, Double-Blind Study. Journal of Oral and Maxillofacial Surgery 78 (2020): 52-62.
- Yagiela JA, Dowd FJ, Neidle EA. Pharmacology and Therapeutics for Dentistry. (5th edtn), St. Louis, Mo: Mosby (2004): 251
- Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc 68 (2002): 546.
- Rahn R, Ball B. Local Anesthesia in Dentistry- Articaine and Epinephrine for Dental Anesthesia (edtn 1), (2001): 44.
- Malamed SF, Gagnon S, Leblanc D. A comparison between articaine HCl and lidocaine HCl in pediatric dental patients. Pediatr Dent 22 (2000): 307.
- Power I, Brown DT, Wildsmith JAW. The effects of fentanyl, meperidine and diamorphine on nerve conduction in vitro. Reg Anesth 16 (1991): 204.
- Brau ME, Koch ED, Vogel W, et al. Tonic blocking action of meperidine on Na+ and K+ channels in amphibian peripheral nerves. Anesthesiology 92 (2000): 147
- Scott LJ, Perry CM. Tramadol: a review of its use in perioperative pain. Drugs 60 (2000): 139.
- Grond S, Sablotzki A. Clinical pharmacology of tramadol. Clin Pharmacokinet 43 (2004): 879.
- Pang WW, Mok MS, Chang DP, et al. Local anesthetic effect of tramadol, metoclopramide, and lidocaine following intradermal injection. Reg Anesth Pain Med 23 (1998): 580.
- Altunkaya H, Ozer Y, Kargi E, et al. Comparison of local anaesthetic effects of tramadol with prilocaine for minor surgical procedure. Br J Anaesth 90 (2003): 320.
- Mert T, Gunes Y, Guven M, et al. Comparison of nerve conduction blocks by an opioid and a local anesthetic. European Journal of Pharmacology 439 (2002): 77.
- Guven M, Mert T, Gunay I. Effects of tramadol on nerve action potentials in rat: comparisons with benzocaine and lidocaine. International Journal of Neuroscience 115 (2005): 339.
- Ege B, Calisir M, Al-Haideri Y, et al. Comparison of Local Anesthetic Efficiency of Tramadol Hydrochloride and Lidocaine Hydrochloride. J Oral Maxillofac Surg 76 (2018): 744.