Evaluating the Learning Curve for Subarachnoid Spinal Anesthesia Among Anesthesiology Fellows Using CUSUM Analysis. How Much is Enough?
Putzu M1, Marchesini M2,3*, Latronico N1, Rasulo F1
1Department of Medical and Surgical Specialties, Radiological Sciences and Public Health, University of Brescia, Brescia, Italy
2Department of Anethesia, Critical Care and Pain Medicine, Mater Olbia Hospital, Olbia, Italy
3Division of Anesthesia and Pain Medicine, National Tumor Institute IRCCS Fondazione G. Pascale, Naples, Italy
*Corresponding Author: Marchesini M, Department of Anethesia, Critical Care and Pain Medicine, Mater Olbia Hospital, Olbia, Italy.
Received: 02 July 2025; Accepted:09 July 2025; Published: 23 July 2025
Article Information
Citation: Putzu M, Marchesini M, Latronico N, Rasulo F. Evaluating the Learning Curve for Subarachnoid Spinal Anesthesia Among Anesthesiology Fellows Using CUSUM Analysis. How Much is Enough?. Anesthesia and Critical care 7 (2025): 42-48.
Share at FacebookAbstract
Background: Subarachnoid spinal anesthesia is a critical yet technically challenging procedure in anesthesiology. Despite its importance, limited data are available on the number of attempts required for trainees to achieve competency and proficiency. Cumulative sum (CUSUM) analysis provides a systematic approach to evaluating learning curves and establishing benchmarks for procedural success.
Methods: This study included 39 first-year anesthesiology fellows at the University of Brescia from January 2021 to January 2023. Residents recorded 1,624 spinal anesthesia procedures using an online data collection system. CUSUM analysis was used to evaluate performance trends and determine competency thresholds, defined as “competent” (failure rate ≤ 15%) and “proficient” (failure rate ≤ 10%). Multilevel logistic regression identified factors influencing procedural outcomes.
Results: Data from nine fellows maintaining consecutive records were analyzed. Competency was achieved within 16–153 procedures (median: 39), while proficiency required a mean of 67 procedures. Linear learning trajectories were observed in most residents, although variability existed, with some requiring additional training to stabilize performance. Key factors influencing failure included BMI > 40 (OR = 4.53), poorly palpable interspinous spaces (OR = 2.19–9.43), and sitting position (OR = 0.42). Experience reduced failure rates by 2.63% per additional procedure (p < 0.001).
Discussion: CUSUM analysis effectively tracked learning curves and identified individual progress. Competency benchmarks supported structured training programs, while patient and procedural variables highlighted the need for diverse clinical exposure. Variability among trainees underscored the importance of tailored feedback and support.
Conclusions: Competency in subarachnoid spinal anesthesia is typically achieved after a median of 39 procedures, with proficiency requiring further practice. CUSUM analysis offers a robust framework for optimizing anesthesiology training, enhancing procedural success, and ensuring patient safety.
Keywords
Subarachnoid spinal anesthesia; CUSUM analysis; Learning curve; Anesthesiology training; Procedural competency
Article Details
1. Introduction
Subarachnoid spinal anesthesia is among the most commonly used regional anesthesia techniques, valued for its rapid onset, profound sensory and motor blockade, and cost-effectiveness [1]. It is routinely used in a wide range of surgical procedures, from orthopedic and obstetric interventions to lower abdominal surgeries. However, the precision required to navigate the subarachnoid space and deliver anesthetics to the cerebrospinal fluid makes it a technically demanding procedure [2]. Success depends on a combination of anatomical knowledge, manual dexterity, and situational awareness—skills that take time to develop.
The procedure’s complexity is further compounded by patient-specific factors that can increase difficulty, such as obesity, spinal deformities (e.g., scoliosis, previous surgeries, or degenerative changes), and conditions such as pregnancy that alter spinal anatomy [3]. Additionally, subtle variations in needle choice, patient positioning, and even communication during the procedure can significantly affect outcomes [4,5]. These challenges are particularly daunting for anesthesia fellows, who often face steep learning curves during their training [6].
The path to mastering spinal anesthesia is fraught with difficulties, especially for trainees with limited prior exposure. Errors in technique, such as misidentification of landmarks or inappropriate needle angles, can lead to complications such as failed blocks, post-dural puncture headaches, and nerve injuries [2]. Such complications not only compromise patient safety but also erode trainees’ confidence, further complicating their educational journey. Despite the clinical and educational significance of these challenges, the medical literature remains silent on one pivotal question: How many attempts are required for a fellow to achieve competency in spinal anesthesia? Without objective data, training programs must rely on anecdotal benchmarks, risking inconsistent skill acquisition and variability in clinical outcomes.
Cumulative sum (CUSUM) analysis offers an innovative solution to this challenge, providing a rigorous and systematic approach to evaluating procedural success and learning curves [7]. CUSUM is a statistical tool designed to track performance over time, highlighting deviations from expected outcomes and identifying the inflection point at which consistent competency is achieved. This method has been widely used in fields such as surgery and interventional medicine to determine proficiency thresholds and assess operator performances [8,9]. Its application in regional anesthesia training is particularly promising, as it enables real-time feedback, visual representation of progress, and the identification of factors influencing success or failure [10-13].
This study aimed to leverage CUSUM analysis to evaluate the learning curve of spinal anesthesia among medical fellows. Specifically, we sought to determine the minimum number of procedures required to achieve competence and identify the procedural and patient-related factors influencing success rates. By addressing these critical gaps in the literature, this research could enhance training programs, improve patient outcomes, and establish evidence-based benchmarks for proficiency in spinal anesthesia. It thus contributes to the broader goal of optimizing the educational pathways for future anesthesiologists while ensuring the highest standards of patient care.
2. Materials and Methods
This study was conducted from January 2021 to January 2023 and included 39 first-year anesthesiology fellows at the University of Brescia. The aim was to evaluate the learning curve for subarachnoid spinal anesthesia using CUSUM analysis. Each fellow was instructed to consecutively record every spinal anesthesia procedure they performed using an online data collection form accessible via smartphone. This form was divided into two parts:
- Patient Characteristics: Included variables most likely to predict difficulty, such as previous heavy manual labor (>30 years), prior spinal surgery, poorly palpable interspinous spaces, BMI > 30, and age > 80.
- Procedure Outcome: Recorded the procedure’s outcome, classified as a success or failure, alongside additional characteristics such as independence and technical ease.
For a procedure to be classified as a success, cerebrospinal fluid return was required, with a technical performance score ≤ 2. Points were assigned for
- • Each request for tutor assistance during the procedure.
- • The occurrence of a traumatic or bloody puncture.
CUSUM analysis was used to evaluate performance trends and determine competency thresholds. Two competence levels were analyzed according to the Dreyfus model [14]:
- Competent (p0 = 0.15): Reflecting a moderate failure rate as acceptable, consistent with values used for similar anesthetic procedures.
- Proficient (p0 = 0.10): Representing a higher performance standard, with an acceptable failure rate of 10%.
- CUSUM curves were constructed for each resident, using “constant risk failure charts” due to the absence of literature-based coefficients accounting for variable difficulty. For both levels, the unacceptable failure rate (p1) was set at double the acceptable failure rate (2p0), with Type I and II errors fixed at 0.1 [11].
3. CUSUM Technique Description
CUSUM is a statistical tool originally developed for quality control in industrial processes and later adapted for medical training. It involves plotting the cumulative performance of a process over time, with success or failure events affecting the trajectory. For binary outcomes,
- • Each success reduces the CUSUM score by a calculated “reward” (s).
- • Each failure increases the CUSUM score by a “penalty” (1-s).
- • The method defines two decision limits:
- • h1: Crossing this upper limit indicates performance is “out of control,” suggesting a need for corrective action.
- • h0: Crossing this lower limit confirms the operator has reached the desired competency level.
A multilevel logistic regression analysis was performed to assess the association between independent variables and the probability of failure. This approach was chosen due to the hierarchical data structure, with observations nested within individual physicians. Multilevel regression enables modeling individual-level (patient-level variables) and group-level (physician-level variables) differences, accounting for intra- and inter-group variability.
Independent variables (to be specified: this section will be updated once the model is finalized) were included as fixed effects, while the physician was treated as a random effect to account for potential heterogeneity among physicians. This approach enabled the estimation of the effects of independent variables on outcomes while considering specific differences between physicians.
An alpha level of 0.05 was used to determine statistical significance in all analyses. Statistical analyses were conducted using R software version 4.3.1.
4. Results
Data from 38 residents were analyzed, covering 1,624 procedures. However, only nine residents maintained chronological and consecutive data recording, and their data were included in CUSUM analysis.
3.1 Competency Thresholds
- • Competent Level: Achieved by all nine residents, requiring 16 to 153 procedures (median: 39, mean: 55, SD: 42).
- • Proficient Level: Achieved by 7 of 9 residents, with most reaching this within 100 procedures (mean: 67, median: 67, SD: 31.9).
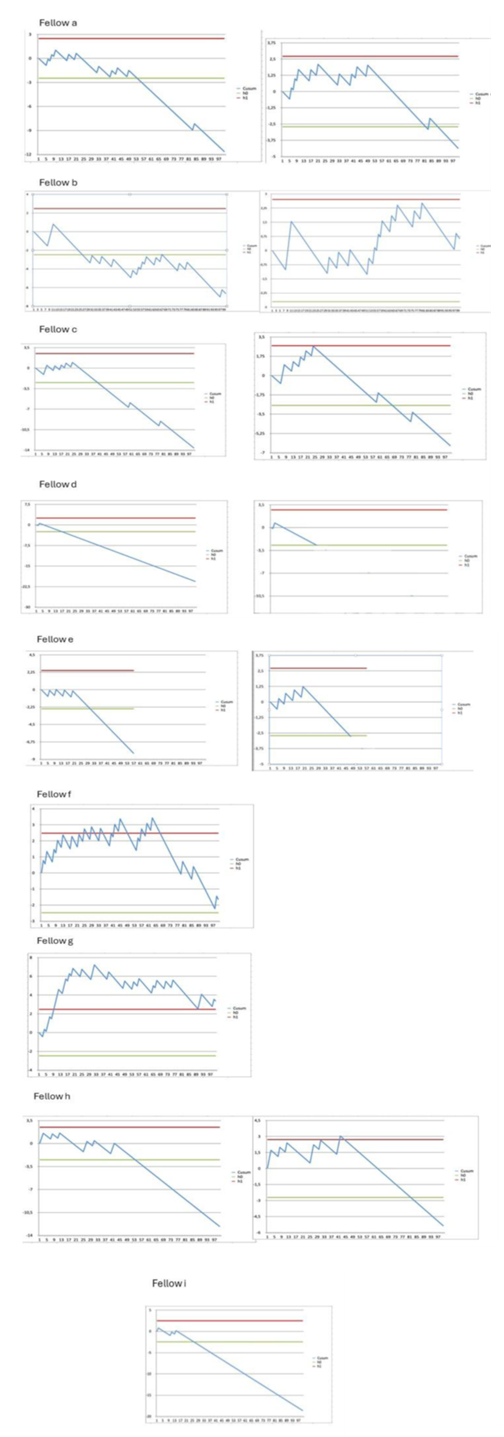
Figure 1 shows the CUSUM graphs for each fellow for the competent and proficient levels (if the competent level is reached within 100 procedures).
3.2 Performance Trends
- • The CUSUM curves showed varying learning trajectories:
- • Linear learning progressions were observed in residents “a,” “b,” “c,” “d,” and “e” without surpassing the upper decision limit (h1).
- • Residents “f” and “g” demonstrated initial instability in their learning curves, crossing h1 multiple times. Resident “f” achieved competence after 70 procedures, while resident “g” required significant additional training and did not complete the proficient level.
A multilevel logistic regression model was used to further investigate the factors influencing the probability of procedural failure (Table 1). The analysis identified several significant variables:
- • Chronological Episode: The failure probability decreased with experience, showing a 2.63% reduction in failure probability with each additional procedure (p < 0.001, OR = 0.9737).
- • BMI > 40: Patients with a BMI > 40 were significantly more likely to experience a failed procedure compared to those with a BMI < 30 (p = 0.044, OR = 4.5278).
- • Heavy Manual Labor: Patients with a history of physically demanding work had an increased failure probability (p = 0.007, OR = 2.5031).
- • Interspinous Space: Poorly or non-palpable interspinous spaces significantly increased failure rates:
- • Non-palpable spaces (p < 0.001, OR = 9.4296).
- • Poorly palpable spaces (p = 0.018, OR = 2.1902).
- • Sitting Position: Procedures performed in the sitting position were less likely to fail compared to the lateral decubitus position (p = 0.021, OR = 0.4181).
- • Traumatic Procedure: Procedures classified as traumatic significantly increased the failure probability (p < 0.001, OR = 58.5627).
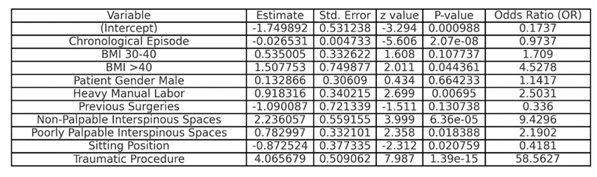
Table 1: Multilevel Logistic Regression Analysis of Predictors of Procedural Failure
3.3 Random Effects
The multilevel logistic regression accounted for variability among residents, with the random effect for the intercept showing a variance of 0.7592 (standard deviation = 0.8713).
These findings confirm that patient-specific factors (e.g., BMI, interspinous space palpability) and procedural characteristics (e.g., sitting position, traumatic maneuvers) are significant in influencing procedural outcomes. The progressive reduction in failure rates with increasing chronological episodes underscores the impact of experience on improving success rates.
4. Discussion
This study highlights the utility of CUSUM analysis in evaluating the learning curve for subarachnoid spinal anesthesia among anesthesiology residents. The findings confirm that competency, as defined by the “competent” level (failure rate ≤15%), is achievable within a range of 16 to 153 procedures, with a median of 39 and a mean of 55. Proficiency, representing a higher standard (failure rate ≤10%), required a mean of 67 procedures. These results provide valuable benchmarks for structuring training programs and assessing trainees’ progress in mastering this essential anesthetic technique.
The linear learning trajectories observed for most residents (“a,” “b,” “c,” “d,” and “e”) suggest consistent skill acquisition without significant deviations indicating poor performance. However, the cases of residents “f” and “g” illustrate the potential for variability in the learning process. Resident “f” showed prolonged instability around the upper decision limit (h1) before demonstrating consistent improvement after 70 procedures. Similarly, resident “g” exhibited persistent difficulty, requiring additional support and training, and failed to reach proficiency despite completing 185 procedures. These findings underline the importance of individualized feedback and targeted interventions for trainees struggling to achieve competence.
Patient-related variables significantly influenced success rates and the learning process. Anatomical challenges, such as poorly palpable interspinous spaces (35.8% of proficient cases), high BMI (24.5%), and previous spinal surgeries, were associated with higher rates of procedural difficulty. These factors highlight the need to expose trainees to a wide range of clinical scenarios during their learning curve to build resilience and adaptability.
This study also underscores the adaptability and precision of CUSUM analysis in tracking procedural success and identifying when performance deviates from acceptable standards. The use of “constant risk failure charts” was particularly effective for monitoring performance in a clinical context, where procedural complexity and patient variability can differ significantly. The method’s ability to flag positive and negative trends offers a valuable tool for ensuring patient safety and optimizing training.
The findings suggest that achieving competency (“competent” level) typically requires a minimum of 60 procedures, consistent with prior studies on similar anesthetic techniques. However, the variability observed among residents indicates that competency thresholds should remain flexible and context-dependent, accounting for individual progress and the complexity of cases encountered.
5. Limitations
Several limitations apply. First, the exclusion of 29 residents due to incomplete or non-consecutive data highlights the challenges of maintaining rigorous data collection in real-world training environments. Additionally, while the study provides clear benchmarks for competency and proficiency, the results may not fully generalize to other institutions with differing patient populations or training protocols. Finally, the reliance on “constant risk failure charts” may not capture the nuances of case-specific challenges, which could be addressed using adjusted risk models in future studies.
Implications for Training Programs
These findings have important implications for anesthesiology education. By identifying specific benchmarks for competency and proficiency, training programs can better structure their curricula, ensuring residents are exposed to sufficient procedural volume and variety. Moreover, using CUSUM analysis can provide real-time feedback, enabling educators to tailor their interventions and support to the needs of individual trainees.
In conclusion, this study demonstrates that subarachnoid spinal anesthesia competency is typically achievable within a median of 39 procedures and that proficiency requires further practice. The integration of CUSUM analysis into training programs represents a valuable step toward standardizing and optimizing the educational process for anesthesiology residents, ultimately enhancing patient safety and care quality.
References
- Di Cianni S, Rossi M, Casati A, et al. Spinal anesthesia: an evergreen technique. Acta Biomed [Internet] 8 79 (2024): 9-17.
- Cook TM, Counsell D, Wildsmith JAW. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists†. Br J Anaesth [Internet] 102 (2009): 179-90.
- Demilie AE, Denu ZA, Bizuneh YB, et al. Incidence and factors associated with failed spinal anaesthesia among patients undergoing surgery: a multi- center prospective observational study. BMC Anesthesiol 24 (2024): 129.
- Gurunathan U, Kunju SM, Hay KE, et al. Usefulness of a visual aid in achieving optimal positioning for spinal anesthesia: A randomized trial. BMC Anesthesiol 18 (2018).
- Pryambodho P, Nugroho AM, Januarrifianto D. Comparison Between Pendant Position and Traditional Sitting Position for Successful Spinal Puncture in Spinal Anesthesia for Cesarean Section. Anesth Pain Med 7 (2017): 14300.
- Guidelines for Fellowship Training in Regional Anesthesiology and Acute Pain Medicine. The Regional Anesthesiology and Acute Pain Medicine Fellowship Directors Group (2010).
- Lin PL, Zheng F, Shin M, et al. CUSUM learning curves: what they can and can’t tell us. Surg Endosc 37 (2024): 7991-9.
- Szymczak P, Grzybowska ME, Sawicki S, et al. Clinical Medicine Laparoscopic Pectopexy-CUSUM Learning Curve and Perioperative Complications Analysis. J Clin Med (2024) https://doi.org/10.3390/jcm10051052.
- Novick RJ, Fox SA, Stitt LW, et al. Direct comparison of risk-adjusted and non-risk-adjusted CUSUM analyses of coronary artery bypass surgery outcomes Surgery for Acquired Cardiovascular Disease Novick et al. J Thorac Cardiovasc Surg 24 (2005): 386-91.
- Naik VN, Devito I, Halpern SH. Cusum analysis is a useful tool to assess resident proficiency at insertion of labour epidurals. Canadian Journal of Anesthesia/Journal canadien d’anesthésie 50 (2003): 694-8.
- De Oliveira Filho GR. The construction of learning curves for basic skills in anesthetic procedures: An application for the cumulative sum method. Anesth Analg [Internet] 95 (2002): 411-6. Available from:
- Kestin IG. A statistical approach to measuring the competence of anaesthetic trainees at practical procedures. Br J Anaesth 75 (1995): 805-9.
- Putzu M, Marchesini M. Ultrasound Block of the Medial Branch. Learning the Technique Using CUSUM Curves. Anesth Essays Res 15 (2021): 385-90.
- Carraccio CL, Benson BJ, Nixon LJ, et al. From the educational bench to the clinical bedside: Translating the Dreyfus developmental model to the learning of clinical skills. Academic Medicine 83 (2008): 761-7.
Related PubMed Articles
- A Comparison of the Lateral Approach (Paramedian) Versus the Modified Lateral Approach (Modified Paramedian) in Spinal Anesthesia: Evaluating Ease of Procedure and Patient Satisfaction in Urological Surgeries; A Triple-Blind Randomized Clinical Trial.
- Effect of preoperative intranasal dexmedetomidine on characteristics of spinal anesthesia with hyperbaric bupivacaine for lower limb orthopedic surgery: a double-blinded randomized control study.
- Neurosurgical Challenges in Recurrent Adhesive Arachnoiditis After Spinal Anesthesia for Cesarean Delivery: Case Report and Literature Review.
- Efficacy of dexmedetomidine with hyperbaric bupivacaine for postoperative analgesia in appendectomy: A randomized controlled trial.
- Comparison of hyperbaric ropivacaine with hyperbaric bupivacaine in subarachnoid block.
- Relationship between neutrophil-lymphocyte ratio and postoperative pain in cesarean section patients done under subarachnoid block: A prospective observational study.
- Ultrasound-assisted technique versus the conventional landmark location method in spinal anesthesia for cesarean delivery in parturients with class 3 obesity: a randomized controlled trial.
- Cervical spinal schwannoma with rapid onset quadriplegia mimicking acute subarachnoid hemorrhage.
- Indications and Technique for Thoracic Segmental Spinal Anesthesia in Clinical Practice: A Narrative Review.