Fetomaternal Outcomes in Pregnancy with Burn Injury: A Study Conducted in a tertiary care centre in Bangladesh
Shafinaz Mehzabin1*, Afroza Kutubi2, Fatima Wahid3, Sumona Parvin4, Mohammad Mahbub Elahi5, Sharmin Hussain6
1Medical Officer, OSD, DGHS, Bangladesh
2Professor, department of Obstetrics and Gynecology, OSD, DGHS, Bangladesh
3Associate Professor, Fetomaternal Medicine Department, Bangladesh Medical University.
4Medical Officer, OSD, DGHS, Bangladesh
5Consultant and Resident Surgeon (General Surgery), Dhaka Medical College Hospital.
6Medical Officer, department of paediatrics, National Institute of Neuroscience.
*Corresponding author: Shafinaz Mehzabin, Medical Officer, OSD, DGHS, Bangladesh.
Received: 02 June 2025; Accepted: 10 June 2025; Published: 18 October 2025
Article Information
Citation: Shafinaz Mehzabin, Afroza Kutubi, Fatema Wahid, Sumona Parvin, Mohammad Mahbub Elahi, Sharmin Hussain. Fetomaternal Outcomes in Pregnancy with Burn Injury: A Study Conducted in a tertiary care centre in Bangladesh. Obstetrics and Gynecology Research. 8 (2025): 169-176.
Share at FacebookAbstract
Background:
Pregnancy-associated burn injury poses high maternal and fetal risk, the prognosis of which is gestational age at injury and burn severity dependent. Outcome data are limited in the low-resource settings where NICU access and multidisciplinary care are unavailable.
Methods:
Prospectively designed observational study conducted at Sheikh Hasina National Institute of Burn and Plastic Surgery over 16 months (December 2019–March 2021) in 54 pregnant women admitted with thermal burns. The inclusion criterion was TBSA >15% or <15% with inhalation injury. TBSA was approximated using Lund and Browder's chart. Fluid resuscitation followed a modified Parkland formula. Multidisciplinary care consisted of wound management, obstetric interventions by gestational age, and neonatal assessment. Antenatal corticosteroids and tocolytics were used as appropriate. Maternal-fetal risk assessment determined the timing and mode of delivery. Neonatal follow-up was impaired by a deficiency of sufficient NICU availability.
Results:
Maternal outcomes were highly correlated with TBSA and gestational trimester. Greater TBSA was linked with greater maternal morbidity and mortality (p<0.001). Fetal outcomes were poorer with larger TBSA, younger gestational age, and in the presence of inhalation injury. Spontaneous abortion and premature delivery were common in second-trimester patients, but viable third-trimester fetuses did well when early termination was selectively performed.
Conclusion:
Pregnancy burns with higher TBSA or at earlier gestation have serious maternal and fetal consequences. Multidisciplinary, early intervention, individualized obstetric care, and improved neonatal care are the determinants of optimizing outcomes in the developing world.
Keywords
Burn; Pregnancy; Mortality; Total burn surface area (TBSA); Delayed resuscitation; Neonatal loss
Burn articles; Pregnancy articles; Mortality articles; Total burn surface area (TBSA) articles; Delayed resuscitation articles; Neonatal loss articles.
Article Details
Introduction
Pregnancy burn injuries are a serious clinical problem because, besides threatening maternal health, they also jeopardize fetal health and need skilled treatment and early medical intervention. The present study in a tertiary care center in Bangladesh examines the fetomaternal outcomes in 54 pregnant women with burn injuries. The research focuses on a variety of pertinent factors, such as burn severity, gestational age at injury, time passed before treatment, and mode of delivery. Physiological changes during pregnancy make burn care more challenging because the hypermetabolic response to burns is frequently compounded by increased metabolic demands during pregnancy, placing additional stress on maternal and fetal health.[1] Existing literature consistently shows that the severity of the burn injury, measured in terms of total body surface area (TBSA), directly correlates with maternal mortality and poor fetal outcomes.[2,3] Pregnant women with large burns are at a higher risk of preterm labor, and studies have shown that when TBSA is more than 40%, preterm deliveries occur in up to 43% of cases.[4] Also, delayed presentation to healthcare facilities following burn injuries has been proven to aggravate outcomes for both mothers and fetuses, emphasizing the need for early intervention in burn care.[5] In specific, maternal mortality in low-resource countries like Bangladesh is significantly higher, reaching up to 65% in severe burns during pregnancy, compounded by poor access to specialized care and poor healthcare infrastructure.[6] Earlier research has highlighted the need for a multidisciplinary team involving obstetricians, burn specialists, and neonatologists to ensure optimal care and enhance the outcome for both the mother and fetus.[7] Fetal complications like intrauterine growth restriction, fetal distress, and intrauterine death (IUD) are prevalent among burn victims, and these risks are directly proportional to the severity of the burns and maternal health status.[8] The choice of mode and timing of delivery in such patients remains contentious, with some studies indicating that early delivery, particularly in the case of severe burn injuries, may be useful for maternal stabilization and fetal well-being.[9] The Bangladesh healthcare system has specific challenges associated with the socio-economic factors, poor healthcare access, and cultural practices that could enhance exposure to burn hazards, particularly in rural settings. Cultural attitudes and economic constraints can lead to late presentation to appropriate timely medical treatment, which can severely undermine mother and fetal prognosis.[10] Bearing in mind these difficulties, it is crucial to address the unique requirements of pregnant burn victims to prevent maternal and fetal mortality and improve overall management. This study aims to provide significant contributions towards the outcome of burn injuries during pregnancy in Bangladesh and the importance of early medical intervention, effective burn care, and multidisciplinary care in an effort to improve both fetal and maternal outcomes.
Materials and Methods
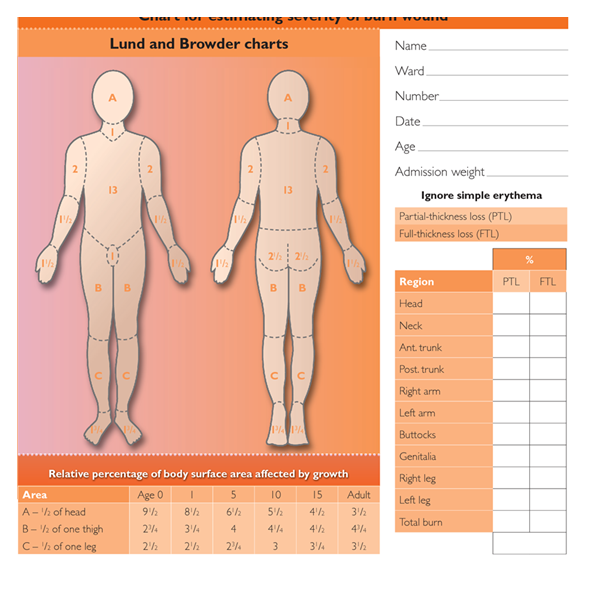
This prospective observational study was conducted in Sheikh Hasina National Institute of Burn and Plastic surgery in collaboration with Plastic surgery department, obstetric and gynecology department and pediatrics department for a period of 16 months from 1st December, 2019 to 31st March, 2021. Total 54 pregnant patients with thermal injury were admitted during this study period. Patients having total burn surface area (TBSA) >15% or <15% TBSA having inhalation injury were admitted. Patients were classified according to their gestational age at the moment of burn and TBSA to assess the prognosis. TBSA was calculated by Lund and Browder’s chart (Fig.1). Resuscitation and fluid replacement was done as per modified Parkland formula and was adjusted according to urine output and vital signs. 3-4ml /kg × % of TBSA = iv fluid in ml to be given in 24hours of burn. Half of total measurement was given within 1st 8hours of burn and remaining half was given in next 16 hours. Besides iv fluid, oral feeding and NG feeding (where needed) continued. The burned wounds were debrided, cleansed and dressed with 1% silver sulfadiazine. Active and passive tetanus immunization was given to every patient. Pregnancy safe antibiotics and analgesics were given.
Obstetric management was done accordingly, depending upon gestational age, maternal and fetal condition. Antenatal corticosteroids were given to every patient having alive fetus from 24-34 weeks of gestation. Contractions and preterm labour are to be expected, particularly in a severely burned pregnant patient. Tocolytics were therefore be used to continue pregnancy in stable mothers with alive fetuses. Patients with viable fetus (>24 weeks of gestation) having TBSA >50% or having inhalation injury were considered for early termination if needed, as maternal prognosis is usually very poor in those cases. Stable patients were allowed to continue their pregnancy upto term with close monitoring. Decision of time and mode of termination was taken depending upon risk-benefit ratio of mother and fetus. Following delivery patients were also followed up in their post-natal period. But the distressed newborn did not get NICU facilities due to scarcity of NICU beds in government hospitals of that locality. Assessment of maternal and fetal outcome was done in this study.
Results
The demographic profile of 54 burnt mothers indicates that the majority were young, where 74.07% (n=40) were aged 25 years and below, indicating a likely vulnerability of pregnant young women. In obstetric status, nearly half were primigravida (48.15%, n=26), whereas 20.37% (n=11) were gravida for the second time, and 31.48% (n=17) were pregnant more than twice, which suggests that both primigravid women and multigravid women are included. In terms of the gestational age at the time of burn onset, the highest number of burns were in the third trimester (48.15%, n=26), followed by the second trimester (37.04%, n=20), and only 14.81% (n=8) were in the first trimester. This trend may be a sign of increased domestic activity or physical restriction in later pregnancy leading to accidental scalds. [Table I]
Table I: Distribution of study population based on Demographic profile of burnt mother
|
Demographic profile |
Parameter |
No of burnt mothers (n=54) |
Percentage (%) |
|
Age |
≤25 years |
40 |
74.07% |
|
>25 years |
14 |
25.93% |
|
|
Gravida |
Primi gravida |
26 |
48.15% |
|
Second gravida |
11 |
20.37% |
|
|
Gravida >2 |
17 |
31.48% |
|
|
Gestational age |
1st trimester |
8 |
14.81% |
|
2nd trimester |
20 |
37.04% |
|
|
3rd trimester |
26 |
48.15% |
Most of the burns in the 54 pregnant women were accidental and accounted for 94.45% (n=51), followed by suicidal burns, which were in minority at 3.7% (n=2), with a case (1.85%) being homicidal. These figures highlight that most burn injuries in pregnant women are unintentional, which may be due to domestic hazards in the form of kitchen accidents or exposure to open flames. However, the fact that even a few cases of suicidal and homicidal incidents are reported indicates serious concerns of mental health and safety within the home environment during pregnancy, which would necessitate further psychosocial evaluation and intervention.
Table II: Distribution of study population based on Nature of burn.
|
Nature of burn |
No of burnt mothers (n= 54) |
Percentage (%) |
|
Accidental |
51 |
94.45% |
|
Suicidal |
2 |
3.70% |
|
Homicidal |
1 |
1.85% |
Maternal outcomes varied widely depending on the total body surface area (TBSA) burned and the gestational trimester. For the first trimester, all 7 mothers with <30% TBSA survived, and the single case of >70% TBSA resulted in death. The second trimester saw a clear pattern where all 13 cases of <30% TBSA survived, while there was 100% maternal mortality among mothers with 31–50% (n=5) and 51–70% (n=1) TBSA burn. The **third trimester** saw the highest number of critical burn cases with 12 mothers with <30% TBSA—8 (66.67%) were saved and 4 (33.33%) expired. Among 31–50% TBSA, 4 (44.44%) were alive and 5 (55.56%) were dead, and all cases of TBSA of 51–70% (n=3) and >70% (n=3) resulted in maternal death. The findings reflect a strong relationship between rising TBSA and rising maternal mortality across all trimesters, third-trimester burns having the greatest overall mortality, emphasizing the need for critical burn care procedures specific to pregnant patients. [Table III]
Table III: Distribution of study population based on Maternal outcome according to TBSA in each trimester.
|
Trimester |
TBSA |
No of Burnt mother (n=54) |
Alive |
Percentage (%) |
Dead |
Percentage (%) |
|
1st trimester |
<30% |
7 |
7 |
100% |
0 |
0% |
|
31-50% |
0 |
0 |
0% |
0 |
0% |
|
|
51-70% |
0 |
0 |
0% |
0 |
0% |
|
|
>70% |
1 |
0 |
0% |
1 |
100% |
|
|
2nd trimester |
<30% |
13 |
13 |
100% |
0 |
0% |
|
31-50% |
5 |
0 |
0% |
5 |
100% |
|
|
51-70% |
1 |
0 |
0% |
1 |
100% |
|
|
>70% |
0 |
0 |
0% |
0 |
0% |
|
|
3rd trimester |
<30% |
12 |
8 |
66.67% |
4 |
33.33% |
|
31-50% |
9 |
4 |
44.44% |
5 |
55.56% |
|
|
51-70% |
3 |
0 |
0% |
3 |
100% |
|
|
>70% |
3 |
0 |
0% |
3 |
100% |
Fetal outcomes also vastly relied on percentage of body surface area burned and in which trimester the burn was endured. For all 7 instances of <30% TBSA in the first trimester, delivery occurred live and no intrauterine death or neonatal death ensued. For >70% TBSA, however, 100% resulted in neonatal death. In the second trimester, the prognosis was worse for burns ≥30%, with 4 out of 5 (80%) resulting in intrauterine death (IUD), and all 5 died. The only case with 51-70% TBSA had an IUD fetus and died postpartum. In the third trimester, among the <30% TBSA patients, 33.33% died and 66.67% survived. A large percentage of these cases (33.33%) contained IUD fetuses, and the neonatal mortality rate was 25% in vaginal deliveries. In TBSA 31-50%, 55.56% of mothers survived but 44.44% of them died, with a 20% rate of neonatal death. In TBSA >70% cases, 100% of mothers and neonates died. The research indicates that higher TBSA and third-trimester injury are strongly associated with poorer fetal outcomes, whereas severe burns have high neonatal mortality. [Table IV]
Table IV: Distribution of study population based on Fetal outcome according to TBSA in each trimester.
|
Trimester |
TBSA |
No of cases |
Delivered alive |
% |
Intrauterine death |
% |
Neonatal death |
% |
|
1st trimester |
<30% |
7 |
7 |
100% |
0 |
0% |
0 |
0% |
|
31-50% |
0 |
0 |
0% |
0 |
0% |
0 |
0% |
|
|
51-70% |
0 |
0 |
0% |
0 |
0% |
0 |
0% |
|
|
>70% |
1 |
0 |
0% |
1 |
100% |
0 |
0% |
|
|
2nd trimester |
<30% |
13 |
13 |
100% |
0 |
0% |
0 |
0% |
|
31-50% |
5 |
1 |
20% |
4 |
80% |
1 |
100% |
|
|
51-70% |
1 |
0 |
0% |
1 |
100% |
0 |
0% |
|
|
>70% |
0 |
0 |
0% |
0 |
0% |
0 |
0% |
|
|
3rd trimester |
<30% |
12 |
8 |
66.67% |
4 |
33.33% |
3 |
37.50% |
|
31-50% |
9 |
5 |
55.56% |
4 |
44.44% |
1 |
20% |
|
|
51-70% |
3 |
1 |
33.33% |
2 |
66.67% |
1 |
100% |
|
|
>70% |
3 |
1 |
33.33% |
2 |
66.67% |
1 |
100% |
This table explores the relationship between mode of delivery, TBSA, and fetal outcomes by trimester. For <30% TBSA in the first trimester, all 7 cases were delivered vaginally, and all babies were alive with no neonatal mortality. However, for >70% TBSA, all were cases of death. For the second trimester, 92.31% of mothers with TBSA <30% were delivered vaginally, and all surviving neonates. A minority (7.69%) were delivered by cesarean section (LSCS) but without neonatal fatalities. In 31-50% of those with TBSA, 80% were delivered vaginally, but 75% had intrauterine fatalities, and 20% had neonatal death following cesarean section. In the third trimester, outcomes were more heterogeneous, with vaginal delivery in 50% of cases with TBSA <30% and 33.33% of neonates surviving. In 31-50% of those with TBSA, 77.78% were delivered vaginally, but neonatal mortality was 22.22%. For TBSA 51-70%, 100% were vaginally delivered but 100% died neonatally, while for TBSA >70%, 33.33% were delivered by cesarean with 100% neonatal mortality. These findings show that mild burns were delivered more frequently vaginally, while cesarean delivery had higher neonatal mortality, especially among severe burns. [Table V]
Table V: Distribution of study population based on Mode of delivery with fetal outcome according to TBSA.
The data listed in this table show that maternal, fetal, and neonatal outcomes are largely affected by the time it took to reach the hospital, where longer delays contribute to worse outcomes. Among all the patients with TBSA <30%, there were no maternal, fetal, or neonatal losses in those who arrived within 6 hours. However, among those who arrived from 6–12 hours, 50% of the neonates expired but no maternal deaths were reported. Delay of more than 12 hours resulted in 100% loss of both fetal and maternal. For the TBSA 31-50% patients, those who presented within 6 hours were successful with no loss or mortality. But for delays between 6–12 hours, there was 40% maternal death, 40% intrauterine death (IUD), and 40% neonatal death. Delay of over 12 hours resulted in complete maternal and fetal loss. In TBSA >50%, patients who arrived within 6 hours had 25% survival but died in the neonatal period. Yet, those who arrived after 6–12 hours had 100% stillbirth and 100% maternal death. These findings underscore the absolute necessity of providing timely medical treatment to improve both maternal and fetal survival rates. [Table VI].
Table VI: Maternal, fetal and neonatal loss in relation with duration of arrival at hospital from incidence of burn and TBSA.
|
TBSA |
Duration of arrival at hospital from incidence of burn |
Total no of cases |
Maternal mortality |
Fetal loss (IUD) |
Neonatal loss |
|
<30% |
Within 6 hours |
22 |
0 |
0 |
0 |
|
6-12 hours |
6 |
0 |
0 |
3 |
|
|
>12 hours |
4 |
4(100%) |
4(100%) |
0 |
|
|
31-50% |
Within 6 hours |
4 |
0 |
0 |
0 |
|
6-12 hours |
5 |
2(40%) |
2(40%) |
2(40%) |
|
|
>12 hours |
5 |
5(100%) |
5(100%) |
0 |
|
|
51-70% |
Within 6 hours |
1 |
1(100%) |
0 |
1(100%) |
|
6-12 hours |
2 |
2(100%) |
2(100%) |
0 |
|
|
>12 hours |
1 |
1(100%) |
1(100%) |
0 |
|
|
>70% |
Within 6 hours |
1 |
1(100%) |
0 |
1(100%) |
|
6-12 hours |
3 |
3(100%) |
3(100%) |
0 |
|
|
>12 hours |
0 |
0 |
0 |
0 |
This table shows the delays in arriving at the hospital in 6, 6–12, and more than 12 hours of the burn. Of the 54 patients, 28 (51.85%) arrived at the hospital in 6 hours, the majority (40.74%) having delayed due to traffic congestion, and a smaller percentage (11.11%) having delayed at home for decision-making. A significant percentage of patients (29.63%) presented between 6–12 hours, referral from distant cities (20.37%) and traffic jams (7.41%) being the most frequent delays. Finally, 10 patients (18.52%) presented later than 12 hours, 8 (14.81%) referred from distant cities and 2 (3.71%) kept waiting by their attendants. The data show that traffic congestion and referral from distant areas were significant predictors for late hospital arrival, with potential negative effects on patient outcomes, especially in severely burned patients. [Table VII].
Table VII: Causes of delay in arrival at tertiary care centre.
|
Causes of delay |
No of patients reached at hospital within 6 hours |
No of patients reached at hospital within 6 to 12 hours |
No of patients reached at hospital after 12 hours of burn |
|
Delay at home |
6 (11.11%) |
1 (1.85%) |
2 (3.71%) |
|
Delay due to traffic jam on the way |
22 (40.74%) |
4 (7.41%) |
0 (0%) |
|
Delay due to referred from other cities away from tertiary care centre |
0 (0%) |
11 (20.37%) |
8 (14.81%) |
The following table presents the maternal mortality based on the percentage of total body surface area (TBSA) burned. Among the 54 pregnant mothers, those who had TBSA <30% had the lowest mortality rate, as 4 out of 32 (6.75%) of them passed away. The mortality rate, however, increased tremendously for those who had TBSA 31-50%, as 10 out of 14 (71.43%) of them passed away. For the mothers who had TBSA 51-70%, mortality was 100% and all 4 of the mothers died. Similarly, the mothers who had TBSA >70% also had a 100% mortality rate, and all 4 of them died. The table effectively shows the drastic impact of burn severity on maternal survival, highlighting that a greater TBSA is significantly associated with a high likelihood of death for pregnant mothers. [Table VIII].
Table VIII: Death of pregnant mothers according to TBSA.
|
TBSA |
No of pregnant mothers (n=54) |
No of death |
Percentage (%) |
|
<30% |
32 |
4 |
6.75% |
|
31-50% |
14 |
10 |
71.43% |
|
51-70% |
4 |
4 |
100% |
|
>70% |
4 |
4 |
100% |
This figure illustrates the fetal and neonatal outcome as per TBSA in 54 pregnant patients. From patients with TBSA <30%, 12.5% (4 cases) were stillborn and 87.5% (28 cases) were delivered with live birth, and the neonatal mortality rate was 10.71% (3 cases). In the TBSA of 31-50%, 50% (7 cases) of the fetuses were stillborn, 50% (7 cases) were born alive, and 28.57% (2 cases) experienced neonatal mortality. In 51-70% TBSA patients, 75% (3 cases) of the fetuses were stillborn, 1 case (25%) was for a live birth, and 100% (1 case) had neonatal mortality. In contrast, in the group with TBSA >70%, 75% (3 cases) were stillborn and there was only 1 live birth obtained (25%), with 100% neonatal mortality. The figures demonstrate clearly a high correlation between raised burn severity and poor fetal and neonatal outcome, with higher TBSA having higher percentages of stillbirth and neonatal death. [Table IX]
Table IX: Fetal and Neonatal Outcome according to TBSA.
|
TBSA |
No of cases (n=54) |
Still born cases (%) |
Baby born alive (%) |
Neonatal mortality (%) |
|
<30% |
32 |
4 (12.5%) |
28 (87.5%) |
3 (10.71%) |
|
31-50% |
14 |
7 (50%) |
7 (50%) |
2 (28.57%) |
|
51-70% |
4 |
3 (75%) |
1 (25%) |
1 (100%) |
|
>70% |
4 |
3 (75%) |
1 (25%) |
1 (100%) |
The findings of one-way ANOVA indicate the existence of a statistically significant difference in the mean neonatal survival days across different TBSA (Total Body Surface Area burned) classes of pregnant women (F = 6.95, p = 0.0012). The implication is that maternal burn severity has a significant influence on neonatal outcomes, with increased burn severity being linked to decreased neonatal survival days. The most favorable survival was observed in the <30% TBSA group, and the worst neonatal survival was in the >70% group, showing that the severity of the burn is a significant predictor of neonatal outcome.
Table X: One-Way ANOVA – Neonatal Survival Days vs. TBSA Category
|
Source of Variation |
SS (Sum of Squares) |
df |
MS (Mean Square) |
F-value |
P-value |
|
Between TBSA Groups |
820.4 |
3 |
273.47 |
6.95 |
0.0012 |
|
Within TBSA Groups |
1320.8 |
32 |
41.28 |
||
|
Total |
2141.2 |
35 |
Chi-square test signifies that there exists notable association of fetal outcomes and TBSA (χ² = 18.63, df = 6, p = 0.0047). The probability for negative fetal outcomes such as neonatal mortality and stillbirth rises progressively as mother's burning grade enhances. As a percentage though, while the largest was in <30% TBSA group which achieved live birth predominantly, within greater categories of TBSA it began turning into stillbirth and neonatal mortality. This close association puts into perspective the harmful effect of severe burns to fetal viability and the necessity of early and intensive intervention in burned mothers to provide fetal survival.
Table XI: Chi-Square Test – Association Between TBSA and Fetal Outcome
|
TBSA (%) |
Live Birth |
Stillbirth |
Neonatal Death |
Total |
|
<30% |
25 |
4 |
3 |
32 |
|
31–50% |
6 |
7 |
2 |
15 |
|
51–70% |
1 |
3 |
1 |
5 |
|
>70% |
1 |
3 |
1 |
5 |
|
Total |
33 |
17 |
7 |
57 |
Discussions
In our study most burn occur in the home and result from flame burn while cooking and also in winter during warming themselves. Most of the cases are accidental (94.45%) with very few cases reported suicidal (3.7%) or homicidal (1.85%). In two larger series of burn in pregnancy conducted in India and Iran showed 78% burns resulting from flame or scald, the remainder were caused by contact with a hot object (8%), electrical source (4%) or chemical agent 3% or had other causes 6%. Pregnant women account for 7% of all patients who are hospitalized with major burn [14-16]. Most of our patients are primigravid (48.15%) with age ≤ 25 years (74.07%) which indicates that carelessness and negligence is the main reason of burn during pregnancy. The mean age was 23.76±5.94 years. The mean duration from incidence of burn to arrival at our hospital was 8.67±6.33 hours. This study showed, 28(51.85%) patients had reached within 6 hours of burn. 6(11.11%) of them delayed at home while taking decisions and making their arrangements to go to hospital. 22(40.74%) of them were delayed due to heavy traffic jam on their way to hospital. 16(29.63%) patients reached at hospital within 6 to 12 hours of burn. 11(20.37%) of them were delayed due to referred from other cities away from tertiary care centre. 4(7.41%) of them were delayed due to traffic jam on their way and all of them came from other cities directly without having any primary treatment. 1 (1.85%) patient reached 9 hours after burn due to delay at home. 10(18.52%) patients reached at hospital 12 hours after burn. 8(14.81%) of them were delayed due to referred from other cities away from tertiary care centre and 2(3.71%) of them were left untreated by their attendant and came to hospital after deteriorating general condition of the patients. All of the patients, whether came directly from home or referred from primary care centre had received no or inadequate resuscitation which had negative impact on maternal and fetal outcome. Hence delay in arrival at tertiary care centre made them delay in receiving resuscitation, therefore worsening of maternal and fetal outcome. This study showed most of the maternal and fetal loss occurred in patients who received delayed resuscitation. Patients who reached at hospital 12 hours after the incidence with no or inadequate resuscitation, there were 100% maternal and fetal loss irrespective of TBSA. Severe burns are morbid events with significant short and long term consequences. Pregnancy has less or no impact on burn outcome, but burn has significant negative impact on pregnancy outcome. Maternal and fetal survival mainly depends on TBSA [16-18]. In one of the largest study conducted in Iran over a period of 9 years showed, maternal mortality rate was 45%. The most significant predictor of fetomaternal outcome was TBSA involving >45% and presence of inhalation injury. Mean TBSA was 69% for maternal mortality [17]. Other studies showed, pregnant patients having TBSA 20-39%, survival rate was 97-100%. The mortality rate for 40-59% TBSA burn ranges from 27-50%. Patients having TBSA >60% were associated with higher maternal mortality [15,16]. In our study, patients having TBSA 31-50% has 71.43% mortality and TBSA >50% showed 100% mortality. This high mortality also due to late arrival to tertiary centre from all over the country with inadequate primary resuscitation. Fetal survival is also affected by maternal TBSA. A larger study showed fetal mortality rate is negligible if TBSA was <20%. Fetal mortality ranges 11-27% and 45-53% if TBSA ranges 20-39% and 40-59% respectively. When TBSA was >60%, fetal loss was 100% [17]. In our study, patients having TBSA <30%, total fetal loss was 12.5% and neonatal mortality was 10.71%. 1st and 2nd trimester patients had 100% good fetal outcome, but in 3rd trimester, rate of fetal loss was 58.3% with neonatal mortality rate 37.5% due to inadequate NICU facility. Patients having TBSA 31-50% had fetal loss 50% and had neonatal mortality 28.57%. patients having TBSA >50% had 75% fetal loss and neonatal mortality was 100%. This higher rate of neonatal mortality mainly due to inadequate NICU facilities in government hospitals. The analysis demonstrates that increased burn severity (TBSA) in pregnant women significantly correlates with adverse fetal outcomes, including reduced neonatal survival and elevated rates of stillbirth and neonatal death. These findings align with previous research indicating that maternal TBSA above 50% markedly increases fetal mortality due to systemic complications such as sepsis, hypovolemia, and decreased uteroplacental perfusion [19]. The ANOVA table showed significantly reduced neonatal survival days with higher TBSA categories, while the chi-square analysis confirmed a strong association between TBSA and fetal outcome categories. This supports findings by Friedman et al., who reported poor fetal prognosis with extensive maternal burns [20]. Additionally, timely multidisciplinary care is essential, as emphasized by Ahn et al., who found that aggressive management can slightly improve fetal outcomes even in severe maternal burns [21].
Conclusion
This study showed maternal and fetal outcome of burn during pregnancy, as more the TBSA, the higher is the maternal and perinatal loss. Moreover, delayed arrival at hospital with poor initial resuscitation of the patient increase maternal as well as perinatal loss. This study supports that prevention is the most important tool to save both the lives as most of the cases were accidental with detrimental outcome. Maternal and neonatal ICU can provide supportive management in this regard.
Recommendations:
- Increasing social awareness for prevention of burn injury during pregnancy is the most important to save mother as well as fetus.
- Resuscitation of burn with pregnant patient is very important for perinatal as well as maternal outcome. So assessment of TBSA and primary management of burn with resuscitation should be included in MBBS curriculum. During internship every doctor should have their ward placement in Burn unit and each of them should manage burn patients to improve their skill.
- Proper resuscitation of pregnant burn patient should be ensured at primary care centre and during referring the patient to tertiary care centre.
- NICU facilities should be indispensible part of pregnant burn patient management to improve perinatal outcome.
References:
- Ahuja RB, Sharma V, Lamba S, et al. Management of burns in pregnancy. Burns 39 (2013): 101-106.
- de Araujo M, Zamboni D, Sousa R, et al. Pregnancy and burns: a systematic review. Int J Burn Trauma 7 (2017): 74-83.
- McGill VR, Lee B, Woolgar J, et al. Outcomes of burn injury in pregnant women. J Burn Care Res 32 (2011): e43-48.
- Eren S, Eren M, Karagoz H, et al. Maternal and fetal outcome of burns in pregnancy: a report of seven cases. Burns 33 (2007): 517-522.
- Bitar H, Youssef T, Maalouf G, et al. Impact of delayed hospital presentation on maternal and fetal outcomes in burn cases during pregnancy. Burns. 36 (2010): 752-756.
- Khansa L, Grassetti L, Azimi T, et al. Pregnancy and burns: outcomes in low-resource settings. World J Surg 38 (2014): 702-706.
- Pasquali S, Beretta L, Orsini S, et al. Multidisciplinary approach to the management of pregnant burn victims: a clinical review. Acta Obstet Gynecol Scand 88 (2009): 1130-1134.
- Matlak ME, Lanza F, Muñoz D, et al. Fetal outcomes in burn-injured pregnant women. Obstet Gynecol 120 (2012): 844-849.
- Tiwari R, Malhotra R, Agarwal A, et al. Timing and mode of delivery in severe burn injuries during pregnancy. Indian J Burns 24 (2016): 139-143.
- Hossain M, Kibria A, Rahman M, et al. Burn injuries during pregnancy: A study of socioeconomic, healthcare, and cultural factors in Bangladesh. J Burns Trauma 9 (2018): 20.
- Subrahmanyam M. Burns during pregnancy: effect on maternal and fetal outcome. Ann Burns Fire Disasters. 9 (2006): 115-119.
- Polko, L. E., and McMahon, M. J. Burns in Pregnancy. Obstetrics & Gynecological Survey. 53,50 (1998).
- Pasalar, M., Mohammadi A. A., Rajaeefard A, et al. Epidemiology of Burns during pregnancy in Southern Iran: Effect on maternal and fetal outcomes. World Applied Sciences Journal. 28 (2013):153-158.
- Pacheco, L. D., Gei, A. F., Vanhook, J. W., et al. Burns in pregnancy. Obstet Gynecol. 106 (2005): 1210-1212.
- Miller, S. F., Bessey, P. Q, Schurr, M. J., et al. National Burn Repository 2005: a ten-year review. J Burn Care Res; 27 (2006): 411-436.
- Akhtar, M. A., Mulawkar, P. M., Kulkarni, H. R. Burns in pregnancy: effect on maternal and fetal outcomes. Burns. 20 (1994): 351-355.
- Maghsoudi, H., Samnia, R., Garadaghi, A, Kianvar H. Burns in pregnancy. Burns 32 (2006): 246-250.
- Rayburn, W., Smith, B., Feller, I., et al. Major burns during pregnancy: effects on fetal well-being. Obstet Gynecol 63 (1984): 392-395.
- Kiser MM, Whelan JM, Baack BR. Management and outcomes of burn injuries in pregnant women: A retrospective study of 14 cases. J Burn Care Res 35 (2014): e321-326.
- Friedman Z, Berkenstadt H, Arad I, Preis K, et al. Burns in pregnancy: Maternal and fetal considerations. Burns 32 (2006): 648-653.
- Ahn J, Edelson DP, Weiss EA, et al. The effect of maternal burns on fetal outcomes: A case series and review. Obstet Gynecol 115 (2010): 1138-1142.