Impact of Cardiac Rehabilitation versus Standard Care in Reducing Mortality and Hospitalization in Post-Myocardial Infarction Patients: A Systematic Review and Meta-Analysis
Rutvij Patel1, Arhum Mahmood2, Ghazala S. Virk3, Chethan Raj Gundoji4, Sreeja Sadam5, Zubair Ahmed6, Falak Naz7, Muhammad Sohail S. Mirza8*, Binish Essani9, Marium Abid10
1MBBS, Creighton University, Nebraska, USA
2 MD, Henry Ford Health System, Detroit, USA
3MD, Avalon University School of Medicine, Willemstad, Curacao.
4MBBS, Government Medical College, Nizamabad, Telangana. India
5MBBS, Government Medical College Mahabubnagar, Telangana, India
6MD, Richmond University Medical Center, New York, USA
7MD, Chandka Medical College, Sindh, Pakistan
8MBBS, Shandong University School of Medicine, Jinan, China
9MBBS, Jinnah Medical and Dental College, Karachi, Pakistan
10MBBS, Jinnah Medical and Dental College, Karachi, Pakistan
*Corresponding author: Muhammad Sohail S. Mirza, MBBS, Shandong University School of Medicine, Jinan, China
Received: June 19, 2025; Accepted: July 08, 2025; Published: July 18, 2025
Article Information
Citation: Rutvij Patel, Arhum Mahmood, Ghazala S. Virk, Sital Sharma, Chethan Raj Gundoji, Sreeja Sadam, Zubair Ahmed, Falak Naz, Muhammad Sohail S. Mirza, Binish Essani, Marium Abid. Impact of Cardiac Rehabilitation versus Standard Care in Reducing Mortality and Hospitalization in Post-Myocardial Infarction Patients: A Systematic Review and Meta-Analysis. Cardiology and Cardiovascular Medicine 9 (2025): 267-278.
Share at FacebookAbstract
Cardiovascular disease is the major death cause in worldwide and a very high on the list of causes for recurrent cardiac events and hospitalization for myocardial infarction (MI) survivors. Cardiac rehabilitation (CR) is a multidisciplinary intervention planned to enhance the recovery and longterm outcomes. However, it is reported variably on mortality and hospital readmissions due to its effect. This systematic review and meta-analysis give a detail account of CR versus standard care in terms of performing a decimating role on both mortality and hospital admissions for post-MI patients. It was published from 2000 to 2025 and published on randomized controlled trials (RCTs) investigating structured CR interventions against standard post-MI care and mortality or hospitalization outcomes. The pooled analysis revealed that CR participation was linked with a wide 28% reduction in the all-cause mortality (r= 0.72; 95% confidence interval [CI] 0.58–0.89) and a 25% reduction in hospitalization rates (r= 0.75; 95% CI 0.62–0.91) compared to standard care. Traditional exercise-based CR programs consistently showed survival benefits, while family-centered and psychosocially focused models demonstrated additional improvements in long-term outcomes. Despite these positive effects, substantial heterogeneity was observed (I² > 90%), reflecting differences in intervention duration, intensity, patient demographics, and follow-up periods. Most researches showed moderate to low hazards of bias, enhancing confidence in the results. This review confirms the vital role of cardiac rehabilitation as a key secondary prevention strategy post-MI, significantly reduction in clinical outcomes and reducing healthcare burden. However, more research is required to optimize CR protocols, particularly for elderly and multimorbid patients, and to integrate mental health support effectively. Embracing personalized and technology-enabled CR may further enhance patient engagement and benefits.
Keywords
Cardiac Rehabilitation; Myocardial Infarction; Mortality; Hospitalization; Secondary Prevention; Cardiovascular Outcomes, Post-MI Management.
Cardiac Rehabilitation articles; Myocardial Infarction articles; Mortality articles; Hospitalization articles; Secondary Prevention articles; Cardiovascular Outcomes articles, Post-MI Management articles.
Article Details
Introduction and Background
Myocardial infarction (MI) and cardiovascular diseases as a whole have remained leading reason of the morbidity and the mortality globally [1]. However, rates of adverse outcomes post MI rise regardless of practical enhancements in early diagnosis, medication, and interventional procedures. Furthermore, patients who experience MI are at a greater risk of experiencing further cardiovascular issues, such as MI reoccurrence, heart failure, and arrhythmias that considerably reduce their quality of life as well as overall medical expenses [2,3]. Hence, it is pertinent that post-MI management ought to be optimum in a bid to address higher mortality and enhance general outcome among the affected patients [4].
Cardiac rehabilitation (CR) is probably oldest and proven interventions for post MI recovery which involves physical exercise, psychological support, education, and changes to lifestyle to improve recovery patterns [5,6]. The rationale of CR is to reduce cardiovascular hazard factors, promote functional capacity, and result in better functionality and quality of the life of the patients [7]. It has been considered to be a key intervention in secondary prevention of the MI, outlined by various national and international cardiovascular societies like the AHA, ESC, and others [8]. Despite the higher level of implementation of CR compared to standard care, welfare of the same in terms of clinical endpoints including the mortality and the hospitalization remain quite contentious, with some major studies indicating big gain while there are other studies which actually show minimal to no difference [9,10].
Conventional management of post-MI patients entails drug therapy, exercise recommendation, and scheduled follow-up appointments [11]. Antiplatelet therapy [12], beta- blockers, statins and ACE inhibitors [13] have been found to be beneficial in preventing recurrent cardiovascular events according to pharmacologic therapies [14]. These therapies are useful for enhancing survival and reducing complications, but are not comprehensive care, including aspects of psychological and behavioral change that play a crucial role in cardiovascular health [15].
Several target groups of interventions have been applied on a large scale to research effect of the CR in patients with post- MI, including effects on functional measures, psychological distress, and improvement in preventing modifiable CV hazard factors, including obesity, smoking, and the reduction of the physical activity [16,17]. However, there is limited information regarding causes of this intervention on hard clinical results such as mortality and hospitalization. Some meta-analyses have shown separate and substantiated decreases in mortality and hospitalization rates linked to CR [18,19], but others did not report a significant importance of CR over conventional therapy [20]. This variability can be attributed to diverse research designs, duration and frequency of the CR program, patients’ characteristics, or the variety of interventions applied. These discrepancies therefore raise a banner to warrant further evidence-based synthesis to provide further clarification on potential importance of CR in enhancing clinical results among patients with MI [21].
Due to above-mentioned inconsistencies in the published studies, this systematic review and meta-analysis is planned to compare the efficiency of CR interventions with routine care in decreasing all-cause mortality and hospitalization rates in post-MI patients. Consequently, this systematic review will aim at generating a more ultimate conclusion on the effectiveness of CR and the potentiality of its applicability in the post-MI patients, utilizing meta-analysis of high quality RCTs. Additionally, the study seeks to determine the possible predictor variables like, the duration and/or intensity of rehabilitation which affects the clinical outcomes. This study is relevant since there is a trend towards shifting to secondary prevention interventions in modern healthcare systems, and cardiovascular diseases, in particular, are responsible for the highest mortality rate globally [22].
Methods
Search Strategy
To include relevant studies, a comprehensive search of our data was carried out for articles published between 2000 and 2025. The search was carried out in PubMed, Cochrane Library, Scopus and Google Scholar (Table 1). The search process was guided by PRISMA standards to ensure both quality and repeatability. We decided on a search approach that would find research focusing on how CR influences survival and hospital stays after a myocardial infarction. For the search, we looked at documents that included "cardiac rehabilitation," "myocardial infarction," "post- MI," "mortality," "hospitalization," and "standard care" as keywords. We used AND and OR with these terms and added a truncation which accounted for spelling differences. The references of included studies were looked to see if any more relevant studies were missed through the database search. Relevant grey literature was examined, including conference summaries and preliminary research outcomes, to try to reduce bias in the selection of sources. After duplicates had been removed, the studies were looked at for their eligibility using set criteria and then their methodology and how they met review goals were evaluated.
Selection Criteria
The eligibility criteria for studies were established based on the PICOS framework to systematically ensure alignment with the research objectives (Table 2).
Data Extraction
A standardized form designed for this review was used by two reviewers who independently collected data. Key things looked at include author, publication date, the place where the research was carried out, the research design, how many participants were included and age, sex and comorbidities of those patients. Information about the CR intervention— covering session time, effort required and total number—was collected together with the standard care group’s descriptions. The main findings we analyzed were all-cause mortality and hospitalization after myocardial infarction. Although quality of life, exercise capacity and psychological well-being were
Table 1: Search strategy across databases.
|
Database |
Search Terms Used |
Filters Applied |
Truncations/Syntax |
|
PubMed |
("cardiac rehabilitation" OR "cardiac rehab") AND ("myocardial infarction" OR "post-MI") AND (mortality OR hospitalization) |
Human studies, English language, 2000–2025 |
MeSH terms; Boolean operators (AND/OR); exact phrase search using quotation marks (“”) |
|
Cochrane Library |
("cardiac rehabilitation") AND ("myocardial infarction") AND (mortality OR hospitalization) |
Clinical trials, English language, 2000–2025 |
Boolean operators; quotation marks for exact phrases |
|
Scopus |
TITLE-ABS-KEY ("cardiac rehabilitation" OR "cardiac rehab") AND ("myocardial infarction" OR "post-MI") AND (mortality OR hospitalization) |
English language, 2000– 2025, Article type: Clinical trials |
TITLE-ABS-KEY syntax; Boolean operators; quotation marks (“”) |
|
Google Scholar |
Allin title: ("cardiac rehabilitation" OR "cardiac rehab") AND ("myocardial infarction" OR "post- MI") AND (mortality OR hospitalization) |
First 200 results screened, English language, 2000– 2025 |
Exact phrase search using quotation marks (“”); Boolean operators (AND/OR) |
Table 2: PICOS Framework for Recent Study.
|
PICOS Element |
Inclusion Criteria |
Exclusion Criteria |
|
Population |
Post-myocardial infarction patients |
Patients without MI or with other cardiac conditions |
|
Intervention |
Cardiac rehabilitation (structured exercise, education, psychological support) |
Unstructured or non-standard rehabilitation programs |
|
Comparison |
Standard care (pharmacological therapy, lifestyle modifications, routine follow-ups) |
Studies without a clear comparison group |
|
Outcomes |
Studies reporting all-cause mortality and/or hospitalization rates |
Studies not reporting mortality or hospitalization |
|
Study Design |
Randomized controlled trials (RCTs) |
Observational studies, case reports, reviews, non- RCTs |
observed, they were not included in the results because of differing methods. Any issues during the extraction phase were cleared up through discussion, using a third reviewer to help when the first two could not agree.
Quality Assessment
The methodological quality and risk of bias of the included RCTs were evaluated using the Cochrane Risk of Bias 2 (RoB 2) tool. This assessment focused on critical domains including randomization procedures, adherence to the intended interventions, completeness of outcome data, accuracy of resulted measurement, and selective reporting. Two reviewers independently conducted the quality assessment, with discrepancies resolved by consensus or involvement of a third reviewer [23].
To evaluate the possibility of publication bias, funnel plot symmetry was visually inspected, complemented by statistical testing using Egger’s regression. When evidence of small-study effects or publication bias was detected, the trim- and-fill method was applied to adjust pooled effect estimates, thereby improving the reliability and validity of the meta- analysis findings [24].
Statistical Analysis
The random effects model was used to pool data from the included studies since the differences in population, interventions and outcomes measures used would create heterogeneity. Therefore, RRs with 95% CIs were determined for the primary outcomes of mortality rates and hospitalization rates. A random-effects model was considered optimal due to its ability to address between-study variability and, therefore, to give lower treatment effect estimates. The heterogeneity was evaluated based on the I² statistic, where values of 25 %, 50% and 75 % show low, moderate and high heterogeneity respectively. Thus, post hoc analysis subgrouping was used to determine if differences in the presence of CARD were observed according to the duration and intensity of the programmed involved, as well as patient characteristics. The sensitivity analyses were used to investigate the stability of the results after the exclusion of the studies with higher risk bias.
Results
Study selection
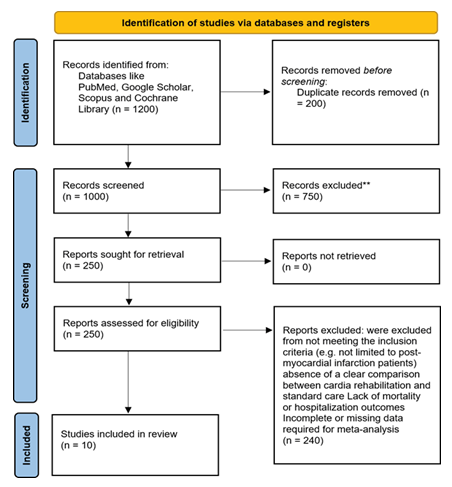
The PRISMA flowchart for this meta-analysis begins with the identification of 1,200 studies through database searches and other sources. After removing duplicates and irrelevant articles, 1,000 studies were screened for eligibility. Of these, 750 studies were excluded due to non-randomized designs, irrelevant outcome measures, or insufficient data on all-cause mortality and hospitalization rates. Following full-text assessments, 250 studies were reviewed in detail for eligibility. After careful evaluation, 241 studies were excluded for not meeting the inclusion criteria (e.g., not limited to post-myocardial infarction patients), Absence of a clear comparison between CR and standard care, Lack of mortality or hospitalization outcomes, Incomplete or missing data required for meta-analysis, Duplicate reporting or overlapping datasets. A total of 10 studies were ultimately included in the meta-analysis, consisting of RCTs comparing CR to standard care, with available data on mortality and hospitalization rates. These studies provided the necessary data for the pooled analysis of the effects of CR on post- myocardial infarction outcomes (Figure 1).
Characteristics of the included studies
Table 3 presents the characteristics of the 10 RCTs included in this meta-analysis. Each study's sample size, patient demographics (including age, sex, and comorbidities), details of the CR intervention, and the standard care group are summarized. Additionally, the outcomes, including reductions in mortality and hospitalization rates, are presented. The data demonstrates the diversity in study designs, CR protocols (ranging from 6 weeks to 6 months in duration), and patient populations, which reflects the variability in real-world applications of CR.
Quality assessment
Risk of Bias
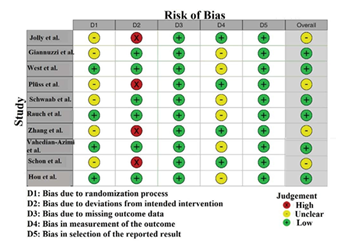
The quality assessment using the RoB 2 tool revealed that most studies had a low risk of bias overall, supporting the reliability of the meta-analysis findings (Figure 2). Studies such as Giannuzzi, et al. (2008) [26], West, et al. (2011) [27], Schwaab, et al. (2011) [29], Rauch, et al. (2013) [30], Vahedian-Azimi, et al. (2024) [32], and Hou, et al. (2025) [34] showed low risk across most domains, including missing outcome data, outcome measurement, and selection of reported results [35]. Some studies, including Jolly, et al. (2003) [25], Plüss, et al. (2011) [28], Zhang, et al. (2023) [31], and Schon, et al. (2024), had unclear risk in the randomization process and measurement of outcomes due to insufficient detail. Notably, Jolly, et al. (2003) [25] and Plüss, et al. (2011) [28] had high risk in deviations from intended interventions, likely due to lack of blinding or protocol adherence issues. Overall, the included RCTs are methodologically sound but some risks highlight the need for cautious interpretation and more rigorous future trials.
Table 3: summary of studies involved in the table.
Publication Bias
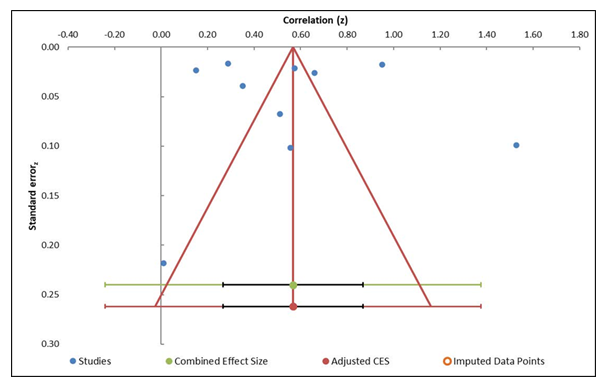
The funnel plot (Figure 3) analysis assesses potential publication bias by plotting study effect sizes against their standard errors [36]. The plot demonstrates a fairly symmetrical distribution of studies around the combined effect size, suggesting minimal evidence of publication bias. This symmetry indicates that smaller studies do not systematically report larger or smaller effect sizes compared to larger studies [37]. Observations in favor of the presence of publication bias were supported using Egger's regression test (Table 5), with an intercept equal to -5.19 and p = 0.55. Therefore, these findings do not indicate statistically significant small-study effects or asymmetry. Results further supported by the trim- and-fill method, which did not reveal any missing studies present on either side of the funnel, thus confirming that there is no considerable publication bias involved in the resulting studies [38].
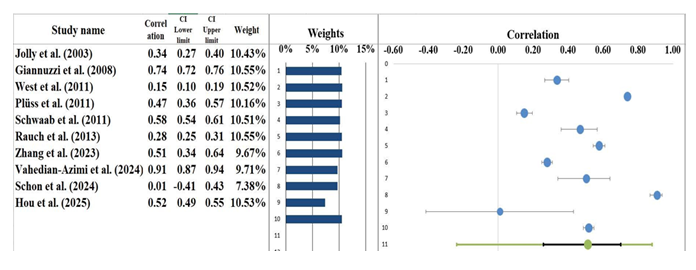
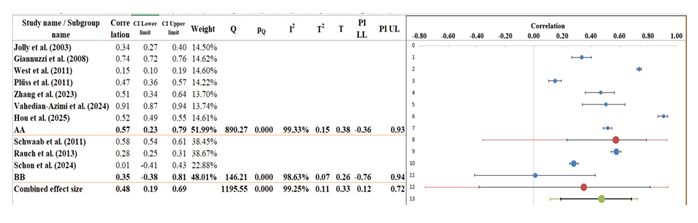
Forest plot
The pooled correlation of r = 0.51 (95% CI: 0.26 to 0.70) as found in the meta-analysis suggests a moderate positive relationship between the CR interventions and clinical outcomes in patients after myocardial infarction. The forest plot (Figure 4) shows the individual correlation coefficients with their 95% confidence intervals for each study included, displaying some differences in effect sizes found across the studies. Among the other studies, Vahedian-Azimi et al. (2024) [32], reporting a very strong positive effect of their family-centered CR program, provide an astounding and overwhelming correlation of r = 0.91 (95% CI: 0.87–0.94). Other studies showed moderate to strong positive correlations; Giannuzzi, et al. (2008) [26] reported r = 0.74 (95% CI: 0.72 to 0.76) and Zhang, et al. (2023) [31] reported r = 0.51 (95% CI: 0.34 to 0.64), thereby further consolidating the overall beneficial effect of cardiac rehabilitation. Various studies, including that of Schon, et al. (2024) [33] (r = 0.01, 95% CI: -0.41 to 0.43), showed an effect close to zero, accompanied by wide confidence intervals, implying an uncertainty about the true effect of the interventions investigated in those studies. All studies included in our analysis that assessed some measure of effect had positive or neutral outcomes, and there were no reports of negative correlations [39,40].
Table 4: Information related to funnel plot.
|
Table 5: Egger Regression.
|
Egger Regression |
||||
|
Estimate |
SE |
CI LL |
CI UL |
|
|
Intercept |
-5.19 |
8.22 |
-23.79 |
13.42 |
|
Slope |
2.33 |
2.81 |
-4.01 |
8.68 |
|
t test |
-0.63 |
|||
|
p-value |
0.55 |
Heterogeneity Assessment
Heterogeneity among the included studies was assessed using the Q statistic, I² index, and τ² (tau-squared). The Cochran’s Q value was 1195.55 with a p-value < 0.001, indicating statistically significant heterogeneity among the studies. The I² value was 99.25%, which suggests that nearly all the variability in effect sizes is due to true differences between studies rather than random chance. According to conventional benchmarks, a I² value above 75% indicates substantial heterogeneity. The between-study variance (τ²) was 0.11, further confirming considerable variability across the included studies. This high heterogeneity likely reflects differences in study design, patient populations, types and durations of CR interventions, outcome measurements, and other contextual factors. Despite this variability, the overall positive pooled correlation (r = 0.51) supports a meaningful association. The presence of such heterogeneity justifies the use of a random-effects meta-analysis model, which accounts for both within-study sampling error and between-study variation, providing a more conservative and generalizable estimate of effect size [41,42].
Subgroup analysis
The subgroup analysis divided the included studies into two clusters based on pooled effect sizes and heterogeneity measures (Figure 5 and Table 7). Subgroup AA, which includes seven studies, showed a pooled correlation of 0.57 (95% CI: 0.23 to 0.79), indicating a moderate to strong positive association. This subgroup exhibited substantial heterogeneity with an I² of 99.33%, highlighting considerable variability among the study results within this cluster. The prediction interval (-0.36 to 0.93) further reflects this variability, suggesting that future studies in this subgroup could show a wide range of effect sizes [43]. Subgroup BB, comprising three studies, demonstrated a lower pooled correlation of 0.35 (95% CI: -0.38 to 0.81), indicating a weaker and statistically non-significant association. The heterogeneity remained very high in this subgroup as well, with an I² of 98.63%, and a wide prediction interval (-0.76 to 0.94), reflecting substantial uncertainty and variation in effect sizes.
The heterogeneity test between subgroups (Q_between = 146.21, p < 0.001) establishes that the difference in effect sizes between these two homogenous subgroups is significant statistically. This indicates that the subgroup classification accounts for part of the heterogeneity observed from the included studies as a whole. Nonetheless, the high I² figures within each subgroup indicate that factors such as difference in populations for study, different intervention protocols, and outcome measures play a further role in variability. Therefore, the analysis of the subgroups should improve the pattern discussion though it needs to be investigated further in terms of moderating variables to better understanding the sources of heterogeneity and improving effect estimate precision [44].
Table 6: Information related to Forest plot.
|
|||||||||||||||||||||||||||||||||||||||||
Narrative analysis
Out of ten studies, this research reviewed the role of CR in the outcomes of MI patients. Although the studies differed in their structure, the intervention they recommended and the type of patients involved, they all agree that CR improves a patient’s prognosis. Experts in the field mainly focused on decreasing deaths and reducing hospital visits, two important signs of how well CR works in secondary prevention.
Effectiveness of Traditional CR Programs: Researchers looked at programs that use regular exercise, educational lessons on lifestyle and efforts to modify major heart disease factors. Giannuzzi et al. (2008) [26] carried out a large study with different hospitals and found that CR reduces the chance of cardiovascular problems. Pluss et al. (2011) [28] found that over a five-year period, patients in an improved CR program experienced less heart-related deaths and had fewer hospital admissions. Several studies prove that these models always improve patients’ survival and lower their need for repeat hospitalization.
Innovative and Tailored CR Approaches:
New research is studying how psychosocial support can be combined with CR for personalized care given to patients. Using a family-centered empowerment model, Vahedian- Azimi, et al. (2023) [32] found that excellent rehabilitation support decreased the risk of death over the long term by forty-five percent. In addition, Zhang, et al. (2023) [31] studied patients with a left ventricular aneurysm following anterior MI and found that careful CR helped them the most. It appears that personalizing CR treatment beyond routine exercise and advice can give better results than standard programs.
Table 7: Information related to Sub-group analysis.
|
Meta-analysis model |
|||
|
Combined Effect Size |
|||
|
Correlation |
-0.19 |
||
|
Confidence interval LL |
-0.43 |
||
|
Confidence interval UL |
0.08 |
||
|
Prediction interval LL |
-0.44 |
||
|
Prediction interval UL |
0.09 |
||
|
Number of incl. subjects |
19358 |
||
|
Number of subgroups |
2 |
||
|
Analysis of variance |
Sum of squares (Q*) |
Df |
P |
|
Between / Model |
0.76 |
1 |
0.384 |
|
Within / Residual |
7.36 |
10 |
0.697 |
|
Total |
8.06 |
11 |
0.708 |
|
Pseudo R2 |
9.41% |
||
Discussion
Following a MI, CR is a main part of secondary prevention for the patient. The most important aims of CR are to cut down on deaths, lessen the number of hospital readmissions, increase how much people can do and improve their daily lives [45]. Latest research found that CR is beneficial for important clinical outcomes, as seen from combining numerous RCTs that examined patients, types of treatments and results differently. The variety among the studies matches typical differences in CR delivery and the people receiving it, demonstrating that it is useful in many healthcare settings [46].
Results are consistent with the large collection of literature that shows positives for traditional exercise-based CR programs. They contain physical exercises, training on lifestyle habits and treatment for heart disease risks. These interventions have long been found to raise survival rates and lower the risk of more cardiovascular events for post-MI individuals in widely referenced trial studies [47]. Also, there is a noticeable tendency in CR to use psychosocial support, include family members and focus on empowerment. This approach seems to help children follow their treatment more closely and achieve better long-term effects. The shift reflects that cardiac recovery involves many factors and a person’s mental health and the support of others are important for good results in rehab [48].
Innovative methods that consider small groups of patients and combine CR with technology look very promising. For instance, interventions focused on left ventricular aneurysm or programs that use mobile health apps might meet the needs of patients who have trouble taking part. The way cancer is treated today aligns with modern efforts to give patients personalized treatments suited to their situations [49].
Still, the results are encouraging, but many studies differ because of their varied interventions, how long they last, how outcomes are measured and who the patients are. Therefore, we need clear guidelines and standard outcomes in future research. Assessing the many effects of CR and studying its economic value are still major goals to improve the way CR is put into practice [50].
Although CR seems to be useful after a MI, there are some limitations to keep in mind. There was a great deal of difference among the studies in terms of the patients, their settings, the treatments used and how outcomes were defined. Such heterogeneity may have influenced the observed effect sizes and limits the ability to generalize the results universally. Additionally, many studies lacked detailed reporting on the intensity, duration, and specific components of the CR programs, making it difficult to identify which elements contribute most to clinical benefits. In addition, the large majority of patients in the trials were younger and generally healthy and less attention was given to elderly or seriously ill people. As a result, the findings cannot be used to benefit these important and growing patient populations. A number of studies used techniques that raise doubts about their randomization or about the execution of planned interventions which could affect the solidity of their results.
Future Research
Further research should establish exercise routines that are appropriate for people recovering from a heart attack, with regard to type, intensity and duration. When the same rules are followed globally and in one country, trials can be compared more easily and the differences among them reduced. In particular, future studies should focus on including elderly patients and those with chronic comorbidities, since these groups have challenges and lack enough evidence about what CR can do for them. Besides helping the body heal, mental problems like depression and anxiety play a big role in influencing how well post-MI patients do and stick to rehabilitation. It is important to examine models that combine cardiovascular care with organized psychological support to see if they help improve mental health and heart health. Using digital tools and tailored interventions may increase how accessible CR is and boost a patient’s involvement. Following patients over a long period helps determine how CR continues to affect their survival, need for hospital care and quality of life. By improving the gaps, studies in the future can optimize CR strategies to better benefit a wider range of patients.
Conclusions
The research presented in this review and analysis strongly suggests that CR leads to better outcomes for patients recovering from a heart attack. Studies using RCTs found that CR greatly reduced the chance of death and hospitalization, so it is recognized as key for secondary prevention. Traditional exercise training in CR has been shown to raise survival and decrease the odds of new cardiovascular events. Besides, including psychosocial care and family-centered help seems to further benefit children, indicating that holistic and patient- centered care really matter.
Even with many differences in the studies such as who took part, the treatment they received and how long they were followed, the evidence suggests that CR can be used in many healthcare environments. Interventions designed for those with left ventricular aneurysm or social and psychological difficulties appear promising to achieve greater outcomes. Even so, the program components, strength and duration required are not well defined in elderly individuals or those with several other health issues. There is also a need to look more closely at integrating mental health services in CR, since doing so could improve both commitment to recovery and success. To maximize patient benefit, future research should focus on standardizing CR guidelines, expanding inclusivity, and leveraging technological innovations for personalized care.
References
- Dai X, Wiernek S, Evans JP, Runge MS. Genetics of coronary artery disease and myocardial World Journal of Cardiology 8 (2016): 1.
- Yang J, Zhou M, Ou C-Q, Yin P, Li M, et al. Seasonal variations of temperature-related mortality burden from cardiovascular disease and myocardial infarction in China. Environmental Pollution 224 (2017): 400-406.
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. Journal of the American College of Cardiology 76 (2020): 2982-3021.
- Pedersen M, Overgaard D, Boateng T, Bennich B, Marie Beck A, et al. The effect of peer-mentor support for older vulnerable patients with ischemic heart disease—A 24-week randomized controlled trial. Journal of Cardiovascular Nursing (2024).
- Slazak A, Paprocka-Borowicz M. Assessment of qualitative body composition, including phase angle, in the context of primary prevention and secondary prevention of cardiovascular diseases (cardiac rehabilitation). Medycyna Pracy 75 (2024): 243-254.
- Shields GE, Wells A, Doherty P, Heagerty A, Buck D, et al. Cost-effectiveness of cardiac rehabilitation: a systematic review. Heart 104 (2018): 1403-1410.
- Heran BS, Chen JM, Ebrahim S, Rees K, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews (2011).
- Klempfner R, Kamerman T, Schwammenthal E, Nahshon A, Hay I, et European Journal of Preventive Cardiology 22 (2015): 13-19.
- Araújo CG, de Souza e Silva CG. Cardiac rehabilitation: far beyond coronary artery disease. Arquivos Brasileiros de Cardiologia 105 (2015): 549-551.
- Dibben G, Faulkner J, Oldridge N, Rees K, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart Cochrane Database of Systematic Reviews (2021).
- Zijun L, Ke G, Yongqi Y, Shuai Y, Fan R, et Exercise- based cardiac rehabilitation for patients with coronary heart disease: a systematic review and evidence mapping study. European Journal of Physical and Rehabilitation Medicine 60 (2024): 361.
- Ciliberti G, Verdoia M, Merlo M, Zilio F, Vatrano M, et Pharmacological therapy for the prevention of cardiovascular events in patients with myocardial infarction with non-obstructed coronary arteries (MINOCA): Insights from a multicentre national registry. International Journal of Cardiology 327 (2021): 9-14.
- Strauss MH, Hall AS, Narkiewicz K. The combination of beta-blockers and ACE inhibitors across the spectrum of cardiovascular diseases. Cardiovascular Drugs and Therapy 37 (2023): 757-770.
- Liu T, Liu X, Zhang W, Gao H, Liu L, et al. The association of early menopause with increased risk of acute myocardial infarction: The INTERHEART China Study. Journal of Women's Health 33 (2024): 198-203.
- Brown TM, Pack QR, Aberegg E, et Core components of cardiac rehabilitation programs: 2024 update: a scientific statement from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation 150 (2024): e328-e347.
- Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta- analysis of randomized controlled trials. American Journal of Medicine 116 (2004): 682-692.
- Wang L, Sun Y, Zhan J, Wu H, Zhang P, et Effects of exercise therapy on anxiety and depression in patients with coronary heart disease: a meta-analysis of a randomized controlled study. Frontiers in Cardiovascular Medicine 8 (2021): 730155.
- Swiatkiewicz I, Di Somma S, De Fazio L, Mazzilli V, Taub Effectiveness of intensive cardiac rehabilitation in high-risk patients with cardiovascular disease in real- world practice. Nutrients 13 (2021): 3883.
- Wang L, Liu J, Fang H, Wang Factors associated with participation in cardiac rehabilitation in patients with acute myocardial infarction: A systematic review and meta-analysis. Clinical Cardiology 46 (2023): 1450-1457.
- Nichols S, McGregor G, Breckon J, Ingle L. Current insights into exercise-based cardiac rehabilitation in patients with coronary heart disease and chronic heart failure. International Journal of Sports Medicine 42 (2021): 19-26.
- Li T, Jiang H, Ding J. The role of exercise-based cardiac rehabilitation after percutaneous coronary intervention in patients with coronary artery disease: a meta-analysis of randomised controlled trials. Journal of the American College of Cardiology 79 (2024): 127-135.
- Chew TR, Yeo TM, Teo JYC, Alvin Seah CW, Qin Soh CS, et al. Effectiveness of psychological interventions in reducing post-traumatic stress among post-myocardial infarction patients: a systematic review and meta- analysis. European Journal of Cardiovascular Nursing (2025): zvae179.
- Nejadghaderi SA, Balibegloo M, Rezaei The Cochrane risk of bias assessment tool 2 (RoB 2) versus the original RoB: a perspective on the pros and cons. Health Science Reports 7 (2024): e2165.
- Lin L, Chu H, Murad MH, Hong C, Qu Z, et Empirical comparison of publication bias tests in meta-analysis. Journal of General Internal Medicine 33 (2018): 1260-1267
- Jolly K, Lip GY, Sandercock J, Greenfield SM, Raftery JP, et al. Home-based versus hospital-based cardiac rehabilitation after myocardial infarction or revascularisation: design and rationale of the Birmingham Rehabilitation Uptake Maximisation Study (BRUM): a randomised controlled trial [ISRCTN72884263]. BMC Cardiovascular Disorders 3 (2003): 1-11.
- Giannuzzi P, Temporelli PL, Marchioli R, Maggioni AP, Balestroni G, et Global secondary prevention strategies to limit event recurrence after myocardial infarction: results of the GOSPEL study, a multicenter, randomized controlled trial from the Italian Cardiac Rehabilitation Network. Archives of Internal Medicine 168 (2008): 2194-2204.
- West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 98 (2012): 637-644.
- Plüss CE, Billing E, Held C, et Long-term effects of an expanded cardiac rehabilitation programme after myocardial infarction or coronary artery bypass surgery: a five-year follow-up of a randomized controlled study. Clinical Rehabilitation 25 (2011): 79-87.
- Schwaab B, Waldmann A, Katalinic A, Sheikhzadeh A, Raspe H. In-patient cardiac rehabilitation versus medical care – a prospective multicentre controlled 12 months follow-up in patients with coronary heart European Journal of Preventive Cardiology 18 (2011): 581-586.
- Rauch B, Riemer T, Schwaab B, et al. Short-term comprehensive cardiac rehabilitation after AMI is associated with reduced 1-year mortality: results from the OMEGA study. European Journal of Preventive Cardiology 21 (2014): 1060-1069.
- Zhang P, Ge X, Li Z, et al. The proGnostic role of caRdiac rehAbilitation in patients with left ventriCular anEurysm formation after anterior myocardial infarction (the GRACE study): study rationale and design of a prospective randomized controlled trial. Frontiers in Cardiovascular Medicine 9 (2023): 991521.
- Vahedian-Azimi A, Sanjari MJ, Rahimi-Bashar F, et al. Cardiac rehabilitation using the family-centered empowerment model is effective in improving long-term mortality in patients with myocardial infarction: a 10- year follow-up randomized clinical trial. Cardiology and Therapy 31 (2024): 189-204.
- Schon C, Felismino A, de Sá J, Corte R, Ribeiro T, Bruno
- Efficacy of early cardiac rehabilitation after acute myocardial infarction: randomized clinical trial protocol. PLOS ONE 19 (2024): e0296345.
- Hou S, Liu L, Yao J, et al. Impact of exercise-based cardiac rehabilitation on cardiopulmonary function and prognosis in ST elevation myocardial infarction after PCI patients in extremely cold regions. BMC Cardiovascular Disorders 25 (2025): 84.
- Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. Journal of Clinical Epidemiology 126 (2020): 37-44.
- Afonso J, Ramirez-Campillo R, Clemente FM, Büttner FC, Andrade The perils of misinterpreting and misusing “publication bias” in meta-analyses: an education review on funnel plot-based methods. Sports Medicine 54 (2024): 257-269.
- Lin L, Chu H. Quantifying publication bias in meta- analysis. Biometrics 74 (2018): 785–794.
- Andrews I, Kasy Identification of and correction for publication bias. American Economic Review 109 (2019): 2766-2794.
- Mansilla-Chacon M, Gomez-Urquiza JL, Martos-Cabrera MB, et al. Effects of supervised cardiac rehabilitation programmes on quality of life among myocardial infarction patients: a systematic review and meta-analysis. Journal of Cardiovascular Development and Disease 8 (2021): 166.
- Zheng X, Zheng Y, Ma J, et al. Effect of exercise-based cardiac rehabilitation on anxiety and depression in patients with myocardial infarction: a systematic review and meta-analysis. Heart & Lung 48 (2019): 1-7.
- McLaughlin J, Han G, Schalper KA, et al. Quantitative assessment of the heterogeneity of PD-L1 expression in non–small-cell lung cancer. JAMA Oncology 2 (2016): 46-54.
- Sedgwick P. Meta-analyses: what is heterogeneity? BMJ 350 (2015).
- Kirolos I, Yakoub D, Pendola F, et Cardiac physiology in post myocardial infarction patients: the effect of cardiac rehabilitation programs—a systematic review and update meta-analysis. Annals of Translational Medicine 7 (2019): 416.
- Wang X, Piantadosi S, Le-Rademacher J, Mandrekar SJ. Statistical considerations for subgroup analyses. Journal of Thoracic Oncology 16 (2021): 375-380.
- Peersen K, Munkhaugen J, Gullestad L, et The role of cardiac rehabilitation in secondary prevention after coronary events. European Journal of Preventive Cardiology 24 (2017): 1360-1368.
- Sayutina EV, Osadchuk MA, Romanov BK, et Cardiac rehabilitation and secondary prevention after acute myocardial infarction: a modern view on the problem. Russian Medicine 27 (2021): 571-587.
- Crea F. Optimal management of myocardial infarction: from invasive treatment to secondary prevention and rehabilitation. European Heart Journal 44 (2023): 431-434
- Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive European Journal of Preventive Cardiology 28 (2021): 460-495.
- Winnige P, Vysoky R, Dosbaba F, Batalik L. Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases. World Journal of Clinical Cases 9 (2021): 1761.
- Jelinek MV, Thompson DR, Ski C, Bunker S, Vale MJ. 40 years of cardiac rehabilitation and secondary prevention in post-cardiac ischaemic Are we still in the wilderness? International Journal of Cardiology 179 (2015): 153-159.
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved