Impact of Hypertension on Progression and Prognosis in Patients with COVID-19: A Retrospective Cohort Study in 1,031 Hospitalized Cases in Wuhan, China
Tianlu Zhang1, Xingwei He2, Yuxin Du1, Yan Tong1, Xueli Wang3, Weizhong Zhang*,4, Hesong Zeng*,2, Yin Shen*,1,5
1Eye Center, Renmin Hospital of Wuhan University, Wuhan, Hubei, 430060, China
2Department of Cardiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, 430030, China
3Institute of Central China Development, Wuhan University, Wuhan, Hubei, 430064, China
4Shanghai Institute of Hypertension, Ruijin Hospital, Shanghai Jiaotong University, Shanghai, 200025, China
5Frontier Science Center for Immunology and Metabolism, Medical Research Institute, Wuhan University, Wuhan, Hubei, 430071, China
*Corresponding author: Yin Shen, Eye Center, Renmin Hospital of Wuhan University, Wuhan, Hubei, 430060, China
Hesong Zeng, Department of Cardiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, 430030, China
Weizhong Zhang, Shanghai Institute of Hypertension, Ruijin Hospital, Shanghai Jiaotong University, Shanghai, 200025, China
Received: 10 July 2025; Accepted: 17 July 2025; Published: 29 July 2025
Article Information
Citation: Tianlu Zhang, Xingwei He, Yuxin Du, Yan Tong, Xueli Wang, Weizhong Zhang, Hesong Zeng, Yin Shen. Impact of Hypertension on Progression and Prognosis in Patients with COVID-19: A Retrospective Cohort Study in 1,031 Hospitalized Cases in Wuhan, China. Fortune Journal of Health Sciences. 8 (2025): 729-737.
Share at FacebookAbstract
Background: A large proportion of COVID-19 patients with chronic comorbidities have been reported to be in severe conditions with unpromising clinical outcomes. However, whether and how these demographic characteristics and underlying diseases, especially hypertension, influence the progression and prognosis of COVID-19 has not been clarified.
Methods: We included COVID-19 patients who had been admitted to Tongji Hospital (Wuhan, China) from January 27, 2020, to March 8, 2020. Raw data were extracted from electronic medical records and statistically analysed by investigators.
Results: Among 1,031 COVID-19 inpatients in this study, 866 were discharged, and 165 were deceased in the hospital. 73% of 165 deceased patients had chronic comorbidities. Patients with underlying diseases showed a CFR (case-fatality rate) 2.8 times that of patients without. Senility and males were observed to be main risk factors for increased CFR, with OR (odds ratio) being 2.94 (95% CI: 2.00 to 4.33; P<0.001) and 2.47 (95% CI: 1.65 to 3.70; P<0.001), respectively. The OR of cases with composite endpoints for patients with simple hypertension was 1.53 (95% CI: 1.07 to 2.17; P=0.019). Senile patients with hypertension were proven to be at high risk early in the disease. The OR of CFR for hypertensive patients taking calcium channel blockers (CCB) was 0.67 (95% CI: 0.37 to 1.20; P=0.176). Among 271 severe cases without IKF, the OR of CFR was 0.42 (95% CI: 0.18 to 0.99; P=0.046) for patients taking CCB after adjustment.
Conclusions: Hypertension is a risk factor affecting the severity of COVID-19 and plays a critical role in worsening clinical outcomes. Therefore, hypertension management in patients with COVID-19 should be regarded as a major challenge in diagnostic and therapeutic strategies.
Keywords
COVID-19; Comorbidities; Hypertension; Calcium channel blockers; in-hospital case-fatality rate
COVID-19 articles; Comorbidities articles; Hypertension articles; Calcium channel blockers articles; in-hospital case-fatality rate articles
Article Details
Introduction
The infection of COVID-19 has swiftly spread worldwide. The clinical spectrum of COVID-19 patients appears to be wide, ranging from asymptomatic infection to mild, and to critical illness [1, 2]. A significant portion of COVID-19 patients were reported to have at least one underlying complication when admitted to the hospital, with hypertension, diabetes mellitus, and other cardiovascular diseases being the most common [3]. There were about 20% of COVID-19 patients abruptly progressing from mild or normal condition to severe or critical illness, while the critical determinants remain to be identified. For early detection, early prediction, and early treatment, identifying the factors and biological indicators, in particular, those of early warning value for the development of disease progression and prognosis, is critical for clinical decision making and medical resource allocation. In this article, we conducted an in-depth retrospective analysis of COVID-19 inpatients who were received and treated intensively in the early stage of the pandemic. The main aim of our study was to summarize clinical characteristics and monitor the effects of antihypertensive drugs in different hospitalized populations both with and without underlying diseases, and to further explore the factors of great influence on and predictive value of COVID-19 progression and prognosis through the medical history, laboratory indicators, and prognosis outcomes.
Methods
Study design and participants
This retrospective cohort study included 1,031 COVID-19 inpatients from Tongji Hospital, Tongji Medical College of HUST (Huazhong University of Science & Technology), the largest designated hospital in Wuhan, China. All patients were diagnosed with COVID-19 according to the Prevention and Control Scheme for Novel Coronavirus Pneumonia (5th edition) published by the National Health Commission of the People’s Republic of China [4] and WHO interim guidance. A confirmed case of COVID-19 was defined as a positive result of serum antibody or reverse transcriptase-polymerase chain reaction (RT-PCR) assay of nasal or pharyngeal swab specimens. The primary outcome was the occurrence of cases with composite endpoints. The CCIR (case-critically ill rate), CFR (case-fatality rate), and LOS (length of stay) were included in secondary outcomes. The admission date of these hospitalized patients was from January 27, 2020, to March 8, 2020. The final date of the follow-up was March 30, 2020. The study was designed by the investigators and conducted in accordance with the principles of the Declaration of Helsinki. The Institutional Review Board of Tongji Hospital, Wuhan, China, approved this retrospective study, and written informed consent was waived (No. TJ-C20200140). Data was analyzed and interpreted by the authors.
Data collection
We obtained raw data regarding 1,031 hospitalized COVID-19 patients in Tongji Hospital. The demographic data, medical history, clinical symptoms and signs, laboratory findings, chest computed tomography (CT), treatment, and clinical outcomes were extracted from electronic medical records with standardized data collection forms for hospitalized COVID-19 patients. All data were double-checked by two experienced physicians to ensure the accuracy of data collection. Disagreement between these two major reviewers was adjudicated by a third reviewer. The demographic data included age and sex; clinical symptoms and signs included fever, cough, dyspnea, myalgia, diarrhea, chest congestion, heart rate, blood pressure, and oximeter oxygen saturation OOS. Laboratory findings from the laboratory information system consist of the complete blood count, LDH, PT, APTT, Scr, eGFR, ALT, AST, serum albumin, D-dimer, NT-proBNP, TNI, CRP, ESR, IL-6, SARS-CoV-2 IgG, SARS-CoV-2 IgM, and SARS-CoV-2 nucleic acid detection. The chest CT report data were obtained from image acquisition and communication systems. Smoking history and baseline comorbidities (hypertension, DM, CHD, COPD, IKF, stroke, and cancer) were extracted from medical history. Drug use conditions (anti-hypertension drugs, anti-coronary drugs, antiviral drugs, antibiotics, corticosteroids, gamma globulin, and traditional Chinese medicine) and mechanical interventions (non-invasive ventilators, tracheal intubation, ECMO, CRRT) of COVID-19 patients during hospitalization were collected from medical advice. Information about the time from symptom onset to admission to the hospital, severity of illness (normal/severe), and clinical outcomes (discharged or deceased) was obtained from the electronic medical system.
Study definitions
According to the Diagnosis & Treatment Scheme for Novel Coronavirus Pneumonia (Trial 7th edition) published by the National Health Commission of the People’s Republic of China [5], the severity of COVID-19 inpatients was classified into mild, common, severe, and critically ill. ACI (Acute cardiac injury) was diagnosed if serum levels of TNI were more than 0.342 μg/L for males and more than 0.156 μg/L for females. IKF (Impaired kidney function) was diagnosed if eGFR was less than 60 mL/min in the admission examination. The composite endpoint was the occurrence of ACI, IKF, or the use of tracheal intubation. Different groups were divided on the basis of the collected medical history. Patients with hypertension were included in the hypertension group, and patients without hypertension were included in the non-hypertension group. The simple hypertension group referred to patients with hypertension and without diabetes mellitus. The simple diabetes mellitus group referred to patients with diabetes mellitus and without hypertension. The hypertension and diabetes mellitus group referred to patients with both hypertension and diabetes mellitus. The Others group referred to patients without hypertension and diabetes mellitus. Patients without hypertension, DM, CHD, COPD, and cancer were included in the non-underlying disease group [6]. The CCB treatment mainly referred to the use of dihydropyridine long-acting calcium channel blockers during hospitalization.
Statistical analysis
Continuous variables were presented as medians with standard deviation (SD) and compared with the independent sample t-test. Categorical variables were summarized as counts and percentages and compared with the Pearson χ² test. The missing data was removed. We used univariable and multivariable logistic regression models to seek insights into risk factors associated with the incidence of critically ill cases, fatality cases, and composite endpoints. A two-sided α of less than 0.05 was considered statistically significant. All analyses were performed using SPSS (version 21.0) and GraphPad Prism (version 8.4.0) software.
Results
There were 514 patients with chronic comorbidities in a total of 1,031 COVID-19 inpatients, accounting for 50%, two-thirds of whom had one chronic comorbidity. The CFR (23.5%) of patients with chronic comorbidities was 2.8 times that of patients with no underlying disease (8.5%). No difference was observed in CFR among patients with different numbers of chronic comorbidities. There were 866 discharged patients and 165 deceased patients in a total of 1,031 COVID-19 inpatients. The clinical characteristics and prognosis conditions, including demographic data, clinical symptoms and signs, chronic comorbidities, and drug therapy, of these two groups are listed in Table 1. Among deceased patients, 73% had chronic comorbidities (Table 1), 56% (92/165) had hypertension or diabetes mellitus (Supplementary Table 1), 47% had hypertension (Table 1).
Table 1: The comparison of clinical characteristics and prognosis conditions between discharged and deceased patients
|
Total (n=1031) |
Discharged patients (n=866) |
Deceased patients (n=165) |
|
|
Age (SD), y |
60.3 (14.3) |
58.7 (14.2) |
68.4 (12.0) |
|
Female (%) |
493 (47.8) |
448 (51.7) |
45 (27.2) |
|
HR (SD), beats/min |
91.4 (16.9) |
90.5 (16.0) |
96.0 (20.8) |
|
SBP (SD), mmHg |
131.3 (19.0) |
131.0 (18.3) |
132.9 (22.3) |
|
DBP (SD), mmHg |
80.3 (12.2) |
80.4 (11.7) |
79.9 (14.7) |
|
OOS (SD), % |
93.5 (7.7) |
95.1 (4.5) |
84.6 (12.9) |
|
Major symptoms (%) |
|||
|
Fever |
859 (83.3) |
714 (82.4) |
145 (87.8) |
|
Cough |
716 (69.4) |
589 (68.0) |
127 (76.9) |
|
Dyspnea |
265 (25.7) |
172 (19.8) |
93 (56.3) |
|
Myalgia |
137 (13.2) |
123 (14.2) |
14 (8.4) |
|
Diarrhea |
177 (17.1) |
142 (16.3) |
35 (21.2) |
|
Chest congestion |
164 (15.9) |
122 (14.0) |
42 (25.4) |
|
Concomitant underlying diseases (%) |
|||
|
COPD |
39 (3.7) |
21 (2.4) |
18 (10.9) |
|
HTN |
384 (37.2) |
307 (35.4) |
77 (46.6) |
|
DM |
189 (18.3) |
152 (17.5) |
37 (22.4) |
|
CHD |
84 (8.1) |
58 (6.6) |
26 (15.7) |
|
Stroke |
22 (2.1) |
15 (1.7) |
7 (4.2) |
|
Cancer |
29 (2.8) |
15 (1.7) |
14 (8.4) |
|
Smoking history |
105 (10.1) |
69 (7.9) |
36 (21.8) |
|
Number of concomitant underlying diseases (excluding smoking history) (%) |
|||
|
1 |
325 (31.5) |
249 (28.7) |
76 (46.0) |
|
2 |
148 (14.3) |
115 (13.2) |
33 (20.0) |
|
>=3 |
41 (4.0) |
29 (3.3) |
12 (7.3) |
|
With at least one chronic comorbidity |
514 (49.9) |
393 (45.4) |
121 (73.3) |
|
Without any chronic comorbidity |
517 (50.1) |
473 (54.6) |
44 (26.7) |
|
Drug therapy (%) |
|||
|
Antiviral drugs |
902 (87.4) |
777 (89.7) |
125 (75.7) |
|
Antibiotics |
770 (74.6) |
609 (70.3) |
161 (97.5) |
|
Traditional Chinese medicine |
678 (65.7) |
617 (71.2) |
61 (36.9) |
|
CCB |
196 (19.0) |
164 (18.9) |
32 (19.3) |
|
RASI |
62 (6.0) |
54 (6.2) |
8 (4.8) |
|
Statins |
38 (3.6) |
33 (3.8) |
5 (3.0) |
According to Table 1, logistic regression analyses were conducted with factors including the elderly (patients >= 65 years old), males, and a variety of underlying diseases (Supplementary Table 2). All the underlying diseases were revealed to show relations to case fatality except for diabetes mellitus (P>0.05). The multivariable logistic regression analysis still showed the relations between COPD, CHD, stroke, cancer, smoking history, and case fatality after adjustment. The corresponding OR of CFR were 2.69 (95% CI: 1.32 to 5.49; P=0.006), 2.04 (95% CI: 1.18 to 3.55; P=0.011), 2.70 (95% CI: 1.00 to 7.31; P=0.050), 8.01 (95% CI: 3.55 to 18.07; P<0.001), and 2.05 (95% CI: 1.25 to 3.38; P=0.005), respectively, while the OR for hypertensive patients was 1.05 (95% CI: 0.72 to 1.54; P>0.05). The adjusted OR of CFR was 2.94 (95% CI: 2.00 to 4.33; P<0.001) and 2.47 (95% CI: 1.65 to 3.70; P<0.001), respectively, for elderly patients and male patients.
A. The subgroup analysis of prognosis in patients with underlying hypertension and diabetes mellitus
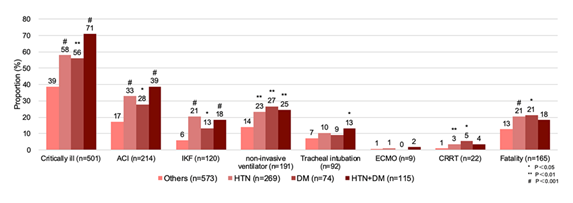
There were 573 patients included in the Others group (Others), 269 in the simple hypertension group (HTN), 74 in the simple diabetes mellitus group (DM), and 115 in the hypertension and diabetes mellitus group (HTN+DM). Multiple indicators, including CCIR, CFR, the incidence of ACI, IKF, and tracheal intubation, the use of non-invasive ventilators, ECMO, and CRRT, were compared among these four groups (Figure 1). The CCIR and CFR were relatively higher in groups with chronic comorbidities. Compared to the Others group, various prognostic indicators were significantly higher in the HTN group and the DM group. Patients in the HTN+DM group showed a higher incidence of ACI, IKF, and tracheal intubation, and the use of non-invasive ventilators.
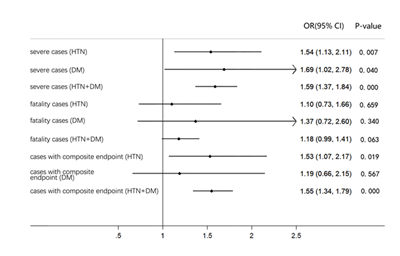
The OR of three major prognostic indicators (incidence of severe cases, fatality cases and cases with composite endpoints) were adjusted by age (Figure 2) in COVID-19 inpatients in the HTN, DM and HTN+DM group, and showed that patients with simple hypertension had higher risk than those with simple diabetes mellitus early in the disease. The OR of occurrence of composite endpoints was 1.53 (95% CI: 1.07 to 2.17; P=0.019) in the HTN group and 1.55 (P<0.001) in the HTN+DM group (Figure 2, Supplementary Table 1). The OR of case fatality was 1.18 (95% CI: 0.99 to 1.41; P=0.063) in the HTN+DM group, indicating its increasing trend in death (Figure 2).
B. The subgroup analysis of case fatality in patients with underlying hypertension
The total of 1,031 COVID-19 inpatients were divided into four groups, ie, the hypertensive discharged group (307 patients), the hypertensive deceased group (77 patients), the non-hypertensive discharged group (559 patients), and the non-hypertensive deceased group (88 patients). The demographic data (age, sex), clinical signs (OOS, HR, SBP, DBP, MAP), and laboratory indicators (NEU, LYM, PLT, CRP, IL-6, LDH, D-dimer, eGFR) were compared among these four groups, as shown in Table 2. There was no significant difference detected between discharged and deceased patients in the hypertension group and the non-hypertension group in sex, OOS, HR, and many other laboratory indicators. However, the eGFR level was significantly lower in the hypertensive deceased group than the non-hypertensive deceased group (66.9±25.7 vs. 78.3±25.9, P=0.005).
Table 2: The comparison of illness conditions of discharged and deceased patients in the hypertension group and the non-hypertension group
P-value 1a: P (hypertension discharged vs. hypertension deceased)
P-value 2b: P (non-hypertension discharged vs. non-hypertension deceased)
P-value 3c: P (hypertension deceased vs. non-hypertension deceased)
Boldface of P-value indicates statistical significance (P<0.05).
C. The subgroup analysis of senility in patients with underlying hypertension
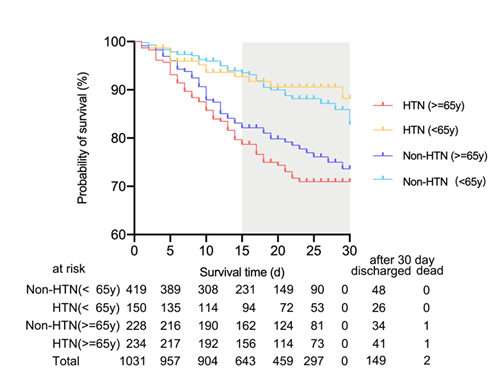
There were 419 patients in the non-hypertensive non-senile group, 150 patients in the hypertensive non-senile group, 228 patients in the non-hypertensive senile group, and 234 patients in the hypertensive senile group, when all patients with hypertension were divided according to age (the age of 65). The demographic data, clinical signs, laboratory indicators, and CCIR, CFR1, and CFR2 were compared among the above four groups (Supplementary Table 3). The results showed that the CCIR in the hypertensive senile group was significantly higher than the non-hypertensive senile group (71% vs. 51%, P<0.001). Different from non-senile patients, senile patients showed significant differences only in the indicators of CRP, LDH, and eGFR between the hypertension group and the non-hypertension group, except for age and blood pressure. By further comparing the probability of survival among the four groups above (Figure 3), we found that the probability of survival in the hypertensive senile group continuously declined from the very start of hospitalization, lowest among the four groups. The CFR of the hypertensive senile group was 26.9%.
D. The subgroup analysis of drug therapy for hospitalized patients
Among all 1,031 hospitalized patients, 196 patients were treated with CCB during hospitalization, and 36 patients deceased (CFR=16%), the same as those not treated with CCB (133/835), while with longer LOS (23.7 vs. 20.8, P=0.001) (Supplementary Table 4). The longer LOS may be associated with more severe conditions before hospitalization in patients treated with CCB. The proportion of the elderly, patients with hypertension, and other underlying diseases was all higher in the CCB group compared to the non-CCB group. No significant difference was found in the proportion of males and the OOS level between patients in these two groups (Supplementary Table 4).
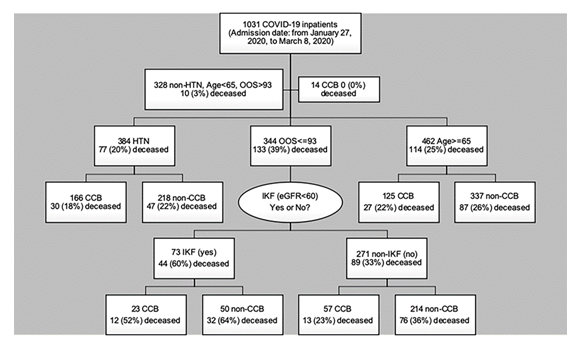
Of 14 patients taking CCB during hospitalization in 328 low-risk cases (cases with non-HTN, age<65y, and OOS>930), no fatality cases occurred (Figure 4), and there was a decreasing trend in LOS (13.2 vs. 17.9, P=0.066) (Supplementary Table 4). The CCB group was observed to show longer LOS across high-risk groups of four different populations (age>=65y; complicated with hypertension; severe cases with IKF; severe cases without IKF), suggesting that patients in these groups were at higher “risk of virus”. However, the CFR of the CCB group in all groupings was relatively lower (Supplementary Table 5).
Among 384 patients with hypertension, 30 of 166 receiving in-hospital treatment of CCB deceased, with a lower CFR compared to the non-CCB group (18% vs. 22%) (Figure 4). By comparing various clinical characteristics between the CCB group and the non-CCB group (Supplementary Table 6), only age, the proportion of patients combining with DM, IKF, and receiving RASI treatment during hospitalization were observed to be significantly different. After adjustment for various relevant factors (age, male, smoking history, DM, IKF, COPD, cancer, RASI) (Supplementary Table 6), the OR of CFR for hypertensive patients in the CCB group was 0.67 (95% CI: 0.37 to 1.20, P=0.176). 57 were treated with CCB during hospitalization, and 13 deceased among 271 severe cases without IKF, with CFR lower than that of the non-CCB group (23% vs. 36%) (Figure 4). The OR of CFR for severe cases without IKF in the CCB group was 0.42 after adjustment for age, sex, and underlying diseases (95% CI: 0.18 to 0.99, P=0.046), which was consistent with the result of an online study with a small sample size (Supplementary Table 7).
Discussion
The clinical manifestations of COVID-19 patients can range from asymptomatic infection to mild, and to critical illness requiring ventilators and even ECMO to sustain life [1, 2]. Wuhan scholars in China first reported that about half of the patients with severe infection were complicated with chronic comorbidities such as hypertension, diabetes mellitus, or coronary heart disease [7]. Among those infected with underlying diseases, about 38% progressed to severe cases [7]. About 60% of severe cases with chronic comorbidities deceased in the hospital [7]. However, whether chronic comorbidities can be regarded as a risk factor affecting the severity of COVID-19 remains controversial at that time. Recently, there were many studies reporting that age and concomitant diseases might aggravate the disease progression and affect clinical outcomes among COVID-19 patients. COVID-19 patients with pre-existing complications were observed to show higher CFR-10.5%, 7.3%, 6.3%, 6.0%, and 5.6% for patients with cardiovascular diseases, diabetes mellitus, chronic respiratory diseases, hypertension, and cancer, respectively [6]. It has been reported that the greater the number of underlying diseases is combined, the greater the severity of COVID-19 [3]. The retrospective analyses of COVID-19 patients in Zhejiang Province and in 31 provinces across mainland China revealed that underlying hypertension was an independent risk factor for severe cases, even after adjustment for age [3, 8]. Among 1,043 COVID-19 patients admitted to the ICU with available data in Italy, 49% had underlying hypertension. After excluding patients still in the ICU as of the deadline of the study, the CFR for patients with and without hypertension was 70% and 47% [9]. The result of the population-based cohort study in England supported that patients with hypertension should be included in the high-risk group [10]. More than that, hypertension was proved to be the only comorbidity associated with the severity of COVID-19 after adjustment for age, sex, and smoking status in a retrospective study in Tongji Hospital with 548 COVID-19 patients included [11].
In our retrospective study, it was found that the determinants of the severity of COVID-19 were closely related to age, male, smoking history, and chronic comorbidities. Chronic comorbidities, such as hypertension and diabetes mellitus, are major risk factors affecting disease progression and prognosis, though they were revealed to show no relations with CFR after adjustment for multiple factors. Patients with simple hypertension may be at higher risk than those with simple diabetes mellitus at the early stage of the disease after adjustment for age, and senile hypertensive patients are at high risk for early progression and prognosis of COVID-19. The CFR of senile hypertensive patients was 26.9%. Why do chronic comorbidities, such as hypertension, increase the risk of disease progression and its prognosis? It was very important and should be investigated. Now, an article named Viral and host factors related to the clinical outcome of COVID-19 was published online [12], to analyze viral genome variation from the sample collection of 326 patients in Shanghai Public Health Center. No significant variation of viral sequences was observed in severe cases of COVID-19, therefore ruling out the possibility of mutation of SARS-CoV-2 itself. Multiple major laboratory indicators were compared among discharged and deceased patients with and without hypertension in our study, with no significant difference observed in general. There was also no significant difference found in SBP and MAP among these four groups. The results suggest that it is likely due to the pathophysiological status and target organ damage in patients with hypertension, such as the RAS system and the laboratory indicator of eGFR, rather than the blood pressure itself, that makes hypertension a risk factor for earlier illness development and prognosis. A single-center study including 417 hospitalized cases in Kuwait published online has found that their dynamic profiling of eGFR in COVID-19 ICU patients highlights the potential role of renal markers in forecasting disease outcome and may identify patients at risk of poor outcome, which is consistent with the results of our study [13].
It is now known that the infection of SARS-CoV-2 needs its combination with ACE2 (angiotensin-converting enzyme 2) and TMPRSS2 (transmembrane serine protease 2) of human alveolar epithelial cells type 2 or other tissues and subsequent replication and multiplication. The amount of virus leads to increased expression of ACE2 in neighboring cells, and then affects macrophages with inflammatory cytokines released [14]. Consequently, the increased expression and activity of ACE2 in tissue could be identified as the critical factor of patients’ susceptibility and disease progression. The Huanggang study, published online, conducted serological tests of ACE2 in 20 COVID-19 patients and 20 non-COVID-19 patients, revealing that the serum level of ACE2 increased 12 hours after infection and remained high 48 hours after infection [15]. ACE2 is only mildly expressed in the lung tissue of healthy humans. However, Brazilian researchers recently found that the expression of ACE2 in the lung tissue was up-regulated in COVID-19 patients with underlying diseases [16], including hypertension, which might provide a reasonable explanation for the increased severity in some COVID-19 patients with underlying complications.
In this retrospective study, we provided the clinical data of COVID-19 inpatients at the early stage of the pandemic in the largest designated hospital in Wuhan, China, after the lockdown of Wuhan City on January 23. Besides, this is the only retrospective study distinguishing the clinical outcomes among COVID-19 inpatients with hypertension only, diabetes mellitus only, and both hypertension and diabetes mellitus, revealing differences between these two major underlying diseases more intuitively. In addition to the prognosis indicators of CFR and LOS, indicators of composite endpoints related to the injury of three main target organs of the lung, kidney, and heart were added to the prognostic indicators, which were more consistent with the clinical manifestations of systemic syndromes of COVID-19. Subgroup analyses were performed on patients with underlying hypertension by separately comparing discharged patients and dead patients, and senile patients and non-senile patients, thus indicating several new findings that might be of practical significance for improving clinical pathways. Based on the actual situation in China, we focused on the in-hospital laboratory findings and prognosis of patients with underlying hypertension using CCB, and encouraging results were finally observed.
As early targeted interventions will prevent the disease from further progressing, a reasonable management strategy of hypertension is of great necessity, and might help to improve clinical outcomes in hospitalized COVID-19 patients at high risks. In a previously published retrospective cohort study in Tongji Hospital, Tongji Medical College of HUST focusing on patients admitted after January 14, 2020 [17], there were 75 deceased cases of 306 patients with baseline hypertension (CFR=24.5%). Meanwhile, there was another study conducted in New York City with 384 of 1,366 hypertensive patients deceased until April 4, 2020 (CFR=28.1%) [18]. However, 77 deceased cases occurred among 384 inpatients with hypertension in our retrospective study with CFR being 20.1%, lower than that of the two above studies. The difference might be associated with increased CCB in-hospital treatment according to expert recommendations announced by the Hubei Cardiovascular Internal Medicine Medical Quality Control Center and Wuhan Medical Association Cardiovascular Disease Credit Association on February 1, 2020 [19]. Subgroup analyses of different populations in our study suggested that the main benefit of CCB in-hospital treatment might come from patients in severe conditions on admission. Among 344 severe hospitalized cases with OOS less than 93% (including 93%), 25 of 80 in the CCB group deceased (CFR=31%), and 108 of 264 deceased in the non-CCB group (CFR=41%), which was consistent with the result of an online study with a small sample size. The study indicated a beneficial effect of amlodipine besylate in reducing the CFR of hypertensive patients, with the CFR being 6.8% (3/44) in the amlodipine besylate-treated group compared to 26.1% (12/46) in the non- amlodipine besylate-treated group (P=0.022) [20].
Study limitations
Our retrospective cohort study has some limitations. Firstly, only admission examination for the eGFR level was captured in the collected data, and the overall level of IKF might therefore be underestimated. Secondly, the information about patients prior to admission was not put into the medical history, so it could not be determined whether the patients continued to take or changed the medication during hospitalization. Thirdly, there was no national unified standard for the normal reference values of some laboratory indicators, thus we followed the standards set by the hospital. Finally, the data entry of underlying diseases was based on the inquiries of patients enrolled in the hospital and might be underestimated due to the influence of the awareness rate.
Acknowledgments
We thank all COVID-19 patients for their participation, our colleagues for their assistance, and the funding source (COVID-19 Emergency Response Project of Wuhan Science and Technology Department (2020020201010018)) for their involvement and support.
Conflicts of Interest
The authors declare that they have no conflict of interest with regard to this study.
|
Nonstandard Abbreviations and Acronyms: |
|
|
ACE2 |
Angiotensin-converting enzyme 2 |
|
ACI |
Acute cardiac injury |
|
ALT |
Alanine aminotransferase |
|
APTT |
Activated partial thromboplastin time |
|
AST |
Aspartate aminotransferase |
|
CCB |
Calcium channel blockers |
|
CCIR |
Case-critically ill rate |
|
CDC |
Chinese Center for Disease Control and Prevention |
|
CFR |
Case-fatality rate |
|
CHD |
Coronary atherosclerotic heart disease |
|
COPD |
Chronic obstructive pulmonary disease |
|
COVID-19 |
Coronavirus disease 2019 |
|
CRP |
C-reactive protein |
|
CRRT |
Continuous renal replacement therapy |
|
DBP |
Diastolic blood pressure |
|
DM |
Diabetes mellitus |
|
ECMO |
Extracorporeal membrane oxygenation |
|
eGFR |
Glomerular filtration rate |
|
ESR |
Erythrocyte sedimentation rate |
|
HR |
Heart rate |
|
ICU |
Intensive care unit |
|
IKF |
Impaired kidney function |
|
IL-6 |
Interleukin 6 |
|
LDH |
Lactate dehydrogenase |
|
LOS |
Length of stay |
|
LYM |
Lymphocytes |
|
MAP |
Mean arterial pressure |
|
NEU |
Neutrophils |
|
NT-proBNP |
N-terminal pro-brain natriuretic peptide |
|
OOS |
Oximeter oxygen saturation |
|
PLT |
Platelet |
|
PT |
Prothrombin time |
|
RAS |
Renin-angiotensin-aldosterone system |
|
RASI |
Renin-angiotensin-aldosterone system inhibitors |
|
SARS-CoV-2 IgG |
SARS-CoV-2 Immunoglobulin G |
|
SARS-CoV-2 IgM |
SARS-CoV-2 Immunoglobulin M |
|
SBP |
Systolic blood pressure |
|
Scr |
Serum creatinine |
|
TMPRSS2 |
Transmembrane serine protease 2 |
|
TNI |
Troponin I |
|
WHO |
World Health Organization |
References
- Guan, W. et al. Clinical Characteristics of Coronavirus Disease 2019 in China. The New England journal of medicine 382 (2019): 1708-1720.
- Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 395 (2020): 497-506.
- Guan W, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 55 (2020).
- National Health Commission of the People’s Republic of China. Prevention & Control Scheme for Novel Coronavirus Pneumonia 5th Edition (2020).
- National Health Commission of the People’s Republic of China and National Administration of Traditional Chinese Medicine. Diagnosis & Treatment Scheme for Novel Coronavirus Pneumonia (Trial) 7th Edition (2020).
- Wu Z & McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. Jama (2020).
- Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (London, England) 395 (2020): 1054-1062.
- Yu Shi, et al. Host susceptibility to severe COVID-19: a retrospective analysis of 487 case outside Wuhan. Research Square (2020).
- Grasselli G, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA (2020).
- Banerjee A, et al. Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet (London, England) 395 (2020): 1715-1725.
- Li X, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol 146 (2020): 110-118.
- Zhang, X. et al. Viral and host factors related to the clinical outcome of COVID-19 (2020).
- Alshukry A, et al. Clinical characteristics of Coronavirus Disease 2019 (COVID-19) patients in Kuwait (2020).
- Ziegler CGK, et al. SARS-CoV-2 Receptor ACE2 Is an Interferon-Stimulated Gene in Human Airway Epithelial Cells and Is Detected in Specific Cell Subsets across Tissues (2020).
- Zhang H, et al. Clinical characteristics of 194 cases of COVID-19 in Huanggang and Taian, China. Infection (2020).
- Pinto BG, et al. ACE2 Expression is Increased in the Lungs of Patients with Comorbidities Associated with Severe COVID-19 (2020).
- Yu, C. et al. Clinical Characteristics, Associated Factors, and Predicting COVID-19 Mortality Risk: A Retrospective Study in Wuhan, China. Am J Prev Med 59 (2020): 168-175.
- Richardson S, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with COVID-19 in the New York City Area. Jama 323 (2020): 2052-2059.
- Liao Y, et al. Expert recommendations for management and treatment of cardiovascular diseases under the epidemic situation of novel coronavirus pneumonia in Hubei Province. Journal of Clinical Cardiology (China) 36 (2020): 201-203.
- Zhang L, et al. Calcium channel blocker amlodipine besylate is associated with reduced case fatality rate of COVID-19 patients with hypertension (2020).
© 2016-2026, Copyrights Fortune Journals. All Rights Reserved