Influence of Intraoperative Liberal vs. Conservative Oxygen Administration on Pulmonary Function in Patients Undergoing Spine Instrumentation: A Randomized Control Trial
Ankur Ghimire1, Rajeev Chauhan1, Kajal Jain1, Ankur Luthra1, Vishal Kumar2, Deepy Zohmangaihi3, Shyam Meena1*, Rashi Sarna1
1Department of Anaesthesia and Intensive care, Postgraduate Institute of Medical Education and Research, Chandigarh, India
2Department of Orthopedic surgery, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3Department of Biochemistry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
*Corresponding Author: Dr. Shyam Charan Meena, Additional Professor, Department of Anaesthesia and Intensive care, Institute of Medical Education and Research, Chandigarh, India.
Received: 07 August 2025; Accepted: 18 August 2025; Published: 27 August 2025
Article Information
Citation: Ankur Ghimire, Rajeev Chauhan, Kajal Jain, Ankur Luthra, Vishal Kumar, Deepy Zohmangaihi, Shyam Meena, Rashi Sarna. Influence of Intraoperative Liberal vs. Conservative Oxygen Administration on Pulmonary Function in Patients Undergoing Spine Instrumentation: A Randomized Control Trial. Anesthesia and Critical care 7 (2025): 58-63.
Share at FacebookAbstract
Background: Hospital malnutrition is often overlooked in developing countries, although adequate nutritional support is essential for optimizing patient care. This study aimed to develop and evaluate the effectiveness of an enteral nutrition formulation prepared from local ingredients.
Methods: A prospective study was conducted on 77 adult patients admitted to intensive care. Protein, energy, and immune markers were assessed upon admission, and an enteral diet capable of meeting energy requirements was formulated using local ingredients (corn flour, soybean flour, powdered milk, soybean oil, whole egg, mineral water, sugar, and cocoa powder). This diet was administered within 48 hours of admission. Nutritional reassessment was performed after seven days of enteral feeding. Data were analyzed using R software and GraphPad.
Results: Upon admission, 18%, 13%, and 49% of patients had mild, moderate, and severe protein reserve deficiencies, respectively. Regarding energy reserves, 23% of patients had mild deficiencies, 29% moderate deficiencies, and 22% severe deficiencies. For immune defense loss, the proportions were 3% for mild deficits, 5% for moderate deficits, and 13% for severe deficits. Enteral feeding significantly improved mean albumin concentrations between admission and nutritional reassessment (p = 0.02).
Conclusion: Our formulation provides an effective means of nutritional support for indigent patients in hospital settings.
Keywords
Spine instrumentation; Postoperative pulmonary complications; Oxygen toxicity; PF ratio; Interleukin-6; FiO2
Article Details
1. Introduction
Undoubtedly, Oxygen is the most important component of life and is the most commonly prescribed medication in anesthesia practice, from induction to extubation, in both General anesthesia and Regional. The high inspired oxygen concentration during anesthesia has been used for years now to prevent and treat hypoxemia caused by alveolar hypoventilation, decrease in functional residual capacity, second gas effect, atelectasis and ventilation-perfusion mismatch, which could occur during any phase of anaesthesia. The high inspired oxygen concentration has also been implicated in decreasing the incidence of surgical site infection and post-operative nausea and vomiting. Low tissue oxygen tension results in patients being more susceptible to SSI and to poor incisional healing. It has also been demonstrated that neutrophil bactericidal activity is impaired at low oxygen tension because this activity depends on the generation of superoxide radicals from molecular oxygen [1]. One hypothesis for decreased incidence of postoperative nausea and vomiting (PONV) is that supplemental oxygen improves oxygen partial pressure in ischemic intestinal tissue during abdominal surgery and decrease the release of serotonin [2]. However, the mechanism for decreased incidence of PONV with high inspired oxygen fraction still eludes us.
The advocates of higher inspired concentration of oxygen were further consolidated when, in 2016, WHO gave a recommendation “adult patients undergoing general anaesthesia with tracheal intubation for surgical procedures should receive an 80% fraction of inspired oxygen intraoperatively and, if feasible, in the immediate postoperative period for 2-6 h to reduce the risk of surgical site infection (SSI)” [3].
Regardless of all the different recommendations and demonstrated advantages, it is not without any consequences to use a high inspired fraction of oxygen in patients undergoing general anesthesia. The role of oxygen and its role in generation of free oxygen radicals (a very reactive component named Reactive Oxygen Species, ROS) that can cause potential toxic effects by inducing oxidative reactions that may generate membrane, DNA or protein damages, make the use of the high inspired fraction of Oxygen a double-edged sword. Therefore, we designed this prospective, single-blind, parallel arm, randomized study with allocation ratio of 1:1 and was conducted in the trauma operation theatres and the recovery wards of one of the premier institutes of North India.
2. Materials and Methods
After obtaining approval of the Institute Ethics Committee (INT/IEC/2021/SPL-889, dated: -01/06/2021) and registration with the Clinical Trial Registry of India (CTRI/2021/07/034824), written informed consents were obtained from all the patients. It was proposed that 75 patients who fulfill the following inclusion criteria be enrolled: ASA I-II patients, no concomitant diseases, aged between 18 and 59 years old, undergoing thoracolumbar spine surgeries (below fifth thoracic vertebrae) due to traumatic fractures.
2.1 Group allocation and Blinding:
The patients were randomized to either the Liberal FiO2 group (80% Oxygen with air) or the Conservative FiO2 group (30% FiO2 with air). Computer-generated random numbers contained in opaque, sealed envelopes were used for randomization. It was given to the anesthesiologist who conducted the anesthesia delivery and was involved in the study. The patients were blinded to group allocation and intervention. Hence, single- blinding was ensured in this study. However, the biochemistry studies of IL-6 and CRP were performed by a researcher who was blinded to the group assignment.
2.2 Anesthesia technique:
After reviewing the pre-anaesthesia checkup (PAC), anesthesia was introduced with Propofol 2 mg/kg, Fentanyl 1 mcg/kg and Vecuronium 0.1 mg/kg, following preoxygenation by a tight-fitting mask.
After intubation, the lungs were ventilated with an adjusted fraction of inspired oxygen as per randomization (either 0.3 or 0.8 FiO2 with Air). Subsequently, they received the allocated FiO2 until immediately before extubation, when an adjusted fraction of inspired oxygen of 1.0 was given again. Anaesthesia depth (BIS 40-60) was maintained with Isoflurane, muscle relaxant and Fentanyl (1mcg/kg/hr) by monitoring the BIS values. The prophylactic antibiotic in an adequate dose was given to all enrolled patient as per the protocol of our institute.
The lungs were ventilated with 6-8ml/kg tidal volume, at 12-14 breaths per minute with end tidal CO2 target of 35-45mmHg and PEEP of 5 cm of H2O. PEEP was primarily increased, if hypoxaemia was detected or suspected in order to keep the SpO2 above 94% and the PaO2 above 70mm of Hg. If this step did not improve oxygenation, FiO2 was increased by 10%. The FiO2 was changed to 1 if no improvement was seen in oxygenation with above corrections. Lung recruitment maneuvers were not allowed in the period from preoxygenation to 2 h after extubation. Neuromuscular block was assessed in all patients using train-of-four (TOF) monitoring. Patients were extubated, when they were fully awake and TOF-ratio ≥ 0.90. Perioperative hypothermia was prevented by using warm IV fluids and forced warmed air in all enrolled patients.
For the prevention of PONV, an IV ondansetron 8 mg was given 30 minutes before the end of surgery, while local infiltration with xylocaine at surgical site and 1gm paracetamol were given for postoperative analgesia.
Arterial blood samples for arterial blood gases, PaO2/FiO2 ratio and lactate values were obtained with 2-mL syringes containing heparin from a radial arterial catheter, and were transported immediately and analysed with blood gas analyser within 10 min. The Samples were obtained at following time intervals: Pre induction, at the end of surgery after extubation, 3 hours post extubation and 24 hours post extubation. The hemodynamic variables were monitored and documented throughout the intraoperative period at least half hourly.
All the samples were analyzed for level of biomarkers using a quantitative IL-6 ELISA kit (Diaclone SAS, Besancon Cedex, and France, Assay Range 1.56 pg/ml – 50 pg/ml and Sensitivity 0.81 pg/ml) and CRP ultra-sensitive ELISA kit (CALBIOTECH Inc., standard range 0.005-0.1 mg/L, analytical sensitivity 0.005 mg/L). Both were analysed with a spectrophotometer at a wavelength of 450 nm.
2.3 Statistics:
According to power analysis, at least 28 patients were required in each group to show a difference in P/F ratio with statistical power 90% and confidence interval 95%. It was assumed that at least fifty percent increase or decrease in the PaO2/FiO2 ratio (343±49) as significant in either group. We decided to enrol 75 patients in anticipation of 20% attrition. The sample size was calculated by comparison of Standard Deviations and mean by using Online OpenEpi software.
All data are expressed as mean ± SD with 95 % confidence intervals. The differences between demographic data, after induction, and before extubation values within groups were analyzed with paired t test, and the differences between two groups at different measurement points were analyzed with unpaired t test. Non-homogenously distributed data were compared using the Mann–Whitney U test. P < 0.05 was considered significant. All the analysis was done using SPSS IBM, Utah 20.0 Statistical program (IBM, SPSS Statistics, Chicago, IL, USA).
3. Results
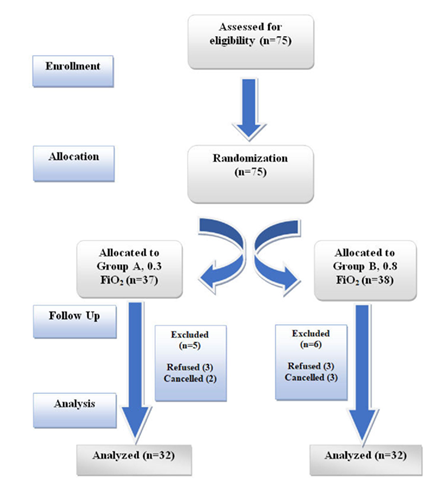
A total of 75 patients (Figure 1: consort diagram), after meeting inclusion criteria were assessed and randomized into 2 groups, out of which 11 patients were excluded (n=64). Three patients in both the groups were excluded after they withdrew their consent for the study, while two patients from 0.3 FiO2 and three patients from 0.8 FiO2 groups were excluded as the surgery was cancelled due to other emergencies.
No significant differences were found in demographic characteristics and perioperative hemodynamic values between groups (Table 1). In both groups, hemodynamic values remained unchanged. All patients were extubated and were sent to the ward without complications.
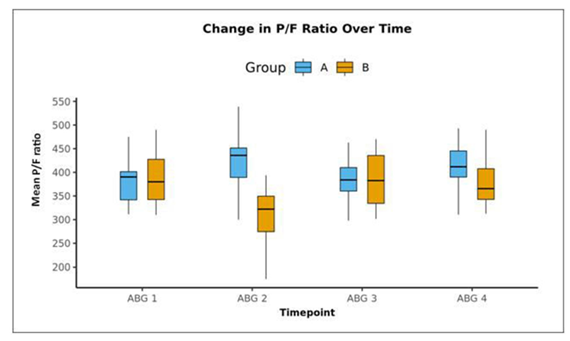
In 0.8 FiO2 group, the PaO2/FiO2 ratio decreased at extubation (Table 2), conversely in 0.3 FiO2 this ratio increased at extubation. There was no difference in PaO2/FiO2 ratios of two groups at baseline, but at extubation PaO2/FiO2 ratios were higher with 0.3 FiO2.
The lactates increased over time in both the groups compared to the baseline values and were higher with 0.8 FiO2 (Table 2); however, two groups did not differ significantly in terms of lactate at any point in time.
|
Basic Details |
Mean ± SD || Median (IQR) || Min-Max || Frequency (%) |
|
Group |
|
|
A |
32 (50.0%) |
|
B |
32 (50.0%) |
|
Age (Years) |
38.22 ± 10.84 || 40.00 (29.75-45.00) || 18.00 - 58.00 |
|
Age |
|
|
18-30 Years |
18 (28.1%) |
|
31-40 Years |
18 (28.1%) |
|
41-50 Years |
20 (31.2%) |
|
51-60 Years |
8 (12.5%) |
|
Gender |
|
|
Male |
53 (82.8%) |
|
Female |
11 (17.2%) |
|
Weight (kg) |
67.86 ± 11.27 || 70.00 (59.00-77.25) || 40.00 - 87.00 |
|
Height (cm) |
165.23 ± 10.81 || 165.00 (157.50-172.00) || 140.00 - 183.00 |
|
BMI (Kg/m²) |
24.81 ± 3.17 || 24.82 (22.37-27.65) || 17.54 - 31.25 |
|
BMI |
|
|
<18.5 Kg/m² |
1 (1.6%) |
|
18.5-22.9 Kg/m² |
18 (28.1%) |
|
23.0-24.9 Kg/m² |
14 (21.9%) |
|
25.0-29.9 Kg/m² |
27 (42.2%) |
|
30.0-34.9 Kg/m² |
4 (6.2%) |
|
Co-Morbidities |
|
|
None |
61 (95.3%) |
|
HTN |
3 (4.7%) |
|
ASA Grade |
|
|
I |
61 (95.3%) |
|
II |
3 (4.7%) |
Table 1: Demographic summary.
|
Group A (0.3 FiO2) |
Group B (0.8 FiO2) |
P value |
|
|
Baseline P/F ratio |
382.31 (42.11) |
386.20 (52.97) |
0.904 |
|
P/F ratio at extubation |
424.69 (53.69) |
315.57 (48.62) |
<0.001 |
|
P/F ratio at 3-hour post extubation |
416.02 (45.54) |
377.96 (52.79) |
0.002 |
|
P/F ratio at 24-hour post extubation |
387.45 (55.18) |
385.16 (52.03) |
0.819 |
|
Lactate baseline |
0.93 (0.47) |
0.93 (0.64) |
0.476 |
|
Lactate after extubation |
1.18 (0.43) |
1.74 (1.93) |
0.082 |
|
CRP Baseline |
0.09 (0.04) |
0.10 (0.04) |
0.074 |
|
CRP after extubation |
0.07 (0.05) |
0.11 (0.04) |
0.001 |
Table 2: PaO2/FiO2 ratio, Lactates (pg/ml) and CRP (mg/L) in both groups (Mean ± SD).
The changes in infection rates on day 1 and 3 did not have any significant results in between groups. The value of CRP increased in 0.8 FiO2 group at extubation while it decreased in 0.3 FiO2 group (Table 2), however the changes were not statistically significant.
In our study, we also tried to compare the pre-operative and post-operative values of Interleukin 6 as a marker for oxidative damage in between the two groups. However, no significant differences were found in between groups at different time points.
4. Discussion
The effect of liberal inspired fraction of oxygen has been debated for ages. Its detrimental effect on physiology of the pulmonary gas exchange due to the collapse of the alveoli that it causes is the major drawback for its use in regular practice. However, the advantages of it decreasing the incidence of surgical site infections and PONV might mandate its use in future. Titration of the liberal inspired fraction of Oxygen in relation to time to deliver only the advantages has been the focus of all the studies done in this niche. In our study, we chose traumatic cases of thoracolumbar spine surgeries done under prone positioning to allow more physiological exchange of gases in the lungs [4].
In both groups, the patients without any preexisting lung pathology were ventilated using the same parameters. Patients in both groups were operated with the same surgical techniques for the same type of surgical pathologies. All these parameters were kept constant. The only variable parameter was the oxygen concentration (80 vs. 30 %). Thus, we have attributed the changes in the clinical condition and biochemical markers (positive and negative) to the oxygen concentration variable.
In our opinion, it is possible that in all the patients that we have recruited, atelectasis was present before induction in room oxygen. However, we did not use any lung recruitment maneuvers and let the physiological status remain the same. After induction, both the groups had a similar PaO2/FiO2 ratio at baseline, indicating homogeneity of the study population.
While no changes in PaO2/FiO2 in baseline was observed, the ratio decreased after an hour in 0.8 FiO2.
At the end of surgery after extubation (Figure 2), the mean (SD) of PaO2/FiO2 Ratio in 0.3 FiO2 and 0.8 FiO2 groups were 424.69 (53.69) and 315.57 (48.62) respectively. The median (IQR) of P/F ratio in 0.3 FiO2 and 0.8 FiO2 group was 435.83 (389.17-451.42) and 322.19 (274.59-349.69) respectively. There was a significant difference between the 2 groups in terms of P/F Ratio (t = 8.522, p = <0.001), with the mean P/F Ratio being highest in 0.3 FiO2 group at extubation. The two groups differed significantly in terms of PaO2/FiO2 Ratio at the following time points: at the end of surgery after extubation and 3 hours post extubation.
In 0.3 FiO2 group, the mean P/F Ratio increased from a minimum of 382.31 at the baseline ABG to a maximum of 424.69 at the extubation, and then decreased to 387.45 at the ABG 24-hour post extubation. This change was statistically significant (Friedman Test: χ2 = 15.9, p = 0.001).
In 0.8 FiO2 group, the mean P/F Ratio decreased from a maximum of 386.20 at the Baseline ABG to a minimum of 315.57 at the extubation, and then increased to 385.16 at the ABG 24-hour post extubation. This change was statistically significant (Friedman Test: χ2 = 23.6, p = <0.001).
This suggests that higher fraction of inspired oxygen might cause increased absorption atelectasis and thus disturb the physiology of gas exchange, as evident from the worsening of P/F ratio over time after intervention. Atelectasis is a common perioperative complication under general anaesthesia. It is observed in more than 90% of all anaesthetized patients with an average of 3-4% collapsed lung area and 10-15% collapsed lung tissue [5]. The P/F ratio in the liberal FiO2 group worsened after intervention and remained status quo till 3 hours after extubation and came to the baseline level after 24 hours. The implication of this finding being, the disturbed physiology likely returned to baseline after 24 hours of stopping the intervention.
However, it is still unclear that from which oxygen concentrations and after what exposure time, the effects start. The lung is first affected because of higher oxygen tension [6]. In rabbits, lung injury developed following exposure to moderate hyperoxaemia at a large tidal volume for 2 hours [7]. In humans, symptoms can occur at 10 hours after initial exposure to hyperoxaemia, although histological changes are apparent earlier [8]. Helmerhorst et al reported that exposure to a high FiO2 for 15 min affected the systemic vascular resistance of patients who had undergone coronary artery bypass grafting surgery [9].
Similarly, the values of Lactate in both the groups increased at the end of surgery. Pre-operative mean value of 0.93 pg/ml in both the groups increased to 1.18 pg/ml and 1.74 pg/ml postoperatively respectively. Both the groups were protected from hypothermia throughout the procedure, and the use of fluid was judicious and comparable in both the groups. None of our patients had documented liver dysfunction which could have affected the clearance of lactate in the body. Under these conditions, it can be well said that the higher rise in lactate value is related in some way with the use liberal FiO2. This issue points out to the need of more studies to uncover the reason.
In a study by Lang et al. [10], they showed that the differences between groups of FiO2 0.4 and 0.7 with respect to the changes in reactive oxygen species and Interleukin 6 were not significant [10]. There was no any incidence of pulmonary complications in any of the groups due to differing FiO2. The markers of oxidative stress, neurological injury or inflammation or pulmonary complications did not rise and no evidences were found that would point to the direction where delivery of higher FiO2 could be blamed.
No significant changes in the levels of Interleukin 6 and CRP were found in our study when compared between baseline values and the values after intervention. Some of the results obtained were invalid. It might be the result of prolonged storage of the sample at -20 C. Due to the logistics issues; the samples were collected, stored and later processed together after the completion of sample size collection.
Schietroma et al. [11] claimed 61 patients (50.8%) had an infection in the 30% FiO2 group and 31 (26%) in the 80% FiO2 group (p < 0.05) [11]. The risk of SSI was 48% lower in the 80% FiO2 group (relative risk 0.51; 95% confidence interval [CI] 0.28–1.08) vs 30% FiO2.
Similarly in our study, only 3 patients from 0.3 FiO2 group were found to have mild erythema (Grade IC, Southampton Wound grading System) and no patients from 0.8 FiO2 group had erythema or any other signs of infection in first day. 9.4% of the participants in the 0.3 FiO2 group had Infection on the 1st Day. On the third day however, 0.3 and 0.8 FiO2 groups had respectively, 1(3.1%) and 2(6.2%) patients who had erythema plus other signs of infection. However, no significant differences between the various groups in terms of distribution of infection on the 1st Day or 3rd Day were found. This probably might have resulted from the antibiotic cover that is routinely given in the patients preoperatively according to our institute protocol.
Treschan et al. [12] in their study found out that the overall postoperative incidence of nausea and vomiting was 41% for inspired oxygen fraction of 0.3 plus placebo, 38% for inspired oxygen fraction of 0.8 plus placebo, and 28% for inspired oxygen fraction of 0.3 plus ondansetron, respectively (P = 0.279) [12]. Therefore, there was no statistically significant difference of PONV incidence among groups.
In our study, 15.6% (5 in 32) and 6.2% (2 in 32) of the participants in the 0.3 and 0.8 FiO2 groups had PONV. There was no significant difference between the various groups in terms of distribution of PONV Score (χ2 = 1.444, p = 0.426). 87.5% and 90.6% of the participants who had PONV in 0.3 and 0.8 FiO2 group had developed it within first 6 hours post operatively.
5. Conclusion
In our study where we used 0.3 and 0.8 FiO2, we found that 0.8 FiO2 decreased the PaO2/FiO2 ratio more and increased the lactated levels compared to 0.3 FiO2. More clinical studies are mandated to further evaluate the effects of higher oxygen fraction.
Conflict of Interest: None.
Funding source: None.
Data availability statement: All of the study relevant data are available with corresponding author and on request to corresponding author.
Authors contributions: AG: Investigation, writing; RC: Review & editing; KJ: Methodology; AL: Review & editing; VK: Data Curation, Methodology; DZ: Investigations; SM: Conceptualization, methodology, original draft writing; RS: Data Curation.
References
- Hopf HW, Hunt TK, West JM, et al. Wound Tissue Oxygen Tension Predicts the Risk of Wound Infection in Surgical Patients. Archives of Surgery 132 (2013): 997-1005.
- Pleuvry BJ. Physiology and pharmacology of nausea and vomiting. Anaesthesia and Intensive Care Medicine 10 (2009): 597-601.
- Allegranzi B, Zayed B, Bischoff P, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. The Lancet Infectious Diseases 16 (2016): e288-e303.
- Johnson NJ, Luks AM, Glenny RW. Gas exchange in the prone posture. Respiratory Care 62 (2018): 1097-1110.
- Magnusson L. New concepts of atelectasis during general anaesthesia. Br J Anaesth 91 (2003): 61-72.
- Bitterman H. Bench-to-bedside review: oxygen as a drug. Crit Care 13 (2009): 205.
- Sinclair SE, Altemeier WA, Matute-Bello G, et al. Augmented lung injury due to interaction between hyperoxia and mechanical ventilation. Crit Care Med 32 (2004): 2496-2501.
- Chawla A, Lavania AK. Oxygen toxicity. Med J Armed Forces India 57 (2001): 131-3.
- Helmerhorst HJF, de Wilde RBP, Lee DH, et al. Hemodynamic effects of short-term hyperoxia after coronary artery bypass grafting. Ann. Intensive Care 7 (2017): 20.
- Lång M, Skrifvars MB, Siironen J, et al. A pilot study of hyperoxemia on neurological injury, inflammation and oxidative stress. Acta Anaesthesiologica Scandinavica 62 (2018): 801-810.
- Schietroma M, Cecilia EM, Santis G De, et al. Supplemental Perioperative Oxygen and Incision Site Infection after Surgery for Perforated Peptic Ulcer: A Randomized, Double-Blind Monocentric Trial 0 (2015): 1-8.
- Treschan TA, Zimmer C, Nass C, et al. Inspired oxygen fraction of 0.8 does not attenuate postoperative nausea and vomiting after strabismus surgery. Anesthesiology 103 (2005): 6-10.
Related PubMed Articles
- The Trendelenburg position decreases the threshold of dynamic variables in predicting fluid responsiveness : A prospective observational study.
- Gas composition and pressure in the hypopharynx during high-flow oxygen therapy through a nasal cannula in healthy volunteers with different breathing patterns.
- Predictive modeling of the performance of the Zoll Z Vent® under hyperbaric conditions.
- T(2)*-weighted oxygen-enhanced pulmonary MRI in COPD is linked to resting and exertional functional measurements.
- Longer daily oxygen use associates with more adverse events, symptoms, and worse health status in long-term oxygen therapy.
- Severe pertussis complicated by pulmonary hypertension in a Moroccan infant: a case report.
- Rituximab induced lung injury.