Lung Ultrasound Predictive Value in Patients with Acute Heart Failure
Harutyun Petrosyan1,2, Anush Manucharyan2, Begimai Iusupbekova2, Anna Terenik2 , Pavel Akulov3, Norik Ghazaryan3*
1MD, Urgent cardiology department, Erebouni Medical Center, Yerevan, Armenia
2MD, Yerevan Scientific Medical center, Yerevan, Armenia
3MD, PHD Independent Physician-Researcher
*Corresponding author:Norik Ghazaryan, MD, PHD, 1129 Linden ave, apt 5, Glendale, CA 91201.
Received: April 10, 2025;Accepted: April 22, 2025;Published: April 25, 2025
Article Information
Citation: Harutyun Petrosyan, Anush Manucharyan, Begimai Iusupbekova, Anna Terenik, Pavel Akulov, Norik Ghazaryan. Lung Ultrasound Predictive Value in Patients with Acute Heart Filure. Cardiology and Cardiovascular Medicine 9 (2025): N111-N113.
Share at FacebookAbstract
Acute heart failure (AHF) is a leading cause of hospitalization globally and is associated with high rates of early readmission and mortality [1]. Pulmonary congestion due to elevated cardiac filling pressures is a hallmark of AHF [2,6], and its timely assessment is critical for guiding therapy and improving outcomes. Traditional tools such as physical examination and chest radiography often fall short in detecting pulmonary congestion early and accurately [2,7]. Lung ultrasound (LUS), particularly through the identification of B-lines— vertical reverberation artifacts indicating extravascular lung water—has emerged as a rapid, non-invasive, and reliable alternative [3,8]. While the diagnostic role of LUS in heart failure (HF) is well established [1,3,8], its prognostic utility, especially in the early phase of AHF, remains underexplored. This study aimed to evaluate whether early B-line assessment using LUS can predict short- and long-term outcomes in patients with acute HF.
Keywords
Lung Ultrasound; Acute Heart Failure
Article Details
Introduction
Acute heart failure (AHF) is a leading cause of hospitalization globally and is associated with high rates of early readmission and mortality [1]. Pulmonary congestion due to elevated cardiac filling pressures is a hallmark of AHF [2,6], and its timely assessment is critical for guiding therapy and improving outcomes.
Traditional tools such as physical examination and chest radiography often fall short in detecting pulmonary congestion early and accurately [2,7]. Lung ultrasound (LUS), particularly through the identification of B-lines—vertical reverberation artifacts indicating extravascular lung water—has emerged as a rapid, non-invasive, and reliable alternative [3,8].
While the diagnostic role of LUS in heart failure (HF) is well established [1,3,8], its prognostic utility, especially in the early phase of AHF, remains underexplored. This study aimed to evaluate whether early B-line assessment using LUS can predict short- and long-term outcomes in patients with acute HF.
Methods
Study Design and Population: This prospective observational study enrolled 194 consecutive adult patients admitted with a diagnosis of acute HF [Table 1].
Inclusion and Exclusion Criteria: Patients aged ≥18 years with confirmed AHF (either de novo or decompensated chronic HF) were included if they underwent LUS within 6 hours of admission. Patients with significant
Table 1: Baseline Characteristics.
|
Characteristic |
Group 1 (<20 B-lines) |
Group 2 (≥20 B-lines) |
p-value |
|
Age (years) |
67.5 ± 12.6 |
66.4 ± 11.7 |
0.53 |
|
Hypertension (%) |
62.2% |
67.7% |
0.42 |
|
Diabetes Mellitus (%) |
30.6% |
29.2% |
0.83 |
|
Prior MI (%) |
71.4% |
71.9% |
0.94 |
|
LVEF (%) |
27.3 ± 5.2 |
26.8 ± 6.4 |
0.55 |
|
Atrial Fibrillation (%) |
37.8% |
36.5% |
0.85 |
|
NT-proBNP (pg/mL) |
3572.6 ± 672.6 |
3754.3 ± 853.6 |
0.10 |
chronic obstructive pulmonary disease (COPD), interstitial lung disease, or conditions impeding LUS imaging were excluded.
Lung Ultrasound Protocol: LUS was performed using a portable ultrasound machine with a convex or phased-array probe. An 8-zone scanning protocol was utilized, assessing anterior and lateral chest regions bilaterally. The total B-line count across all zones was recorded [3,4,8].
Patients were categorized into:
- ⁻ Group 1: <20 B-lines
- ⁻ Group 2: ≥20 B-lines
Clinical and Laboratory Data: Collected data included demographics, comorbidities (e.g., hypertension [AH], diabetes mellitus [DM], prior myocardial infarction [PMI]), left ventricular ejection fraction (LVEF), and presence of atrial fibrillation (AF). NT-proBNP levels were measured at admission and at 12-month follow-up using standardized immunoassays [6].
Outcomes
Primary Outcome:
- ⁻ Change in NT-proBNP from baseline to 12 months Secondary Outcomes:
- ⁻ In-hospital mortality
- ⁻ Requirement for endotracheal intubation
Statistical Analysis: Statistical analysis was conducted using SPSS v26.0. Categorical variables were compared using chi-square tests; continuous variables were analyzed with independent t-tests. A p-value <0.05 was considered statistically significant.
Results
Baseline Characteristics [Table 1]: Baseline demographics and comorbidities were comparable between groups. There was no significant difference in initial NT-proBNP levels (p = 0.10).
NT-proBNP at 12 Months: At 12 months, NT-proBNP
levels were significantly lower in Group 1:
- Group 1: 1324.5 ± 521.4 pg/mL
- Group 2: 1654.7 ± 623.7 pg/mL
- p = 0.0004
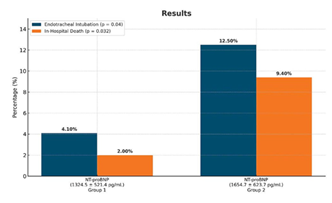
In-Hospital Outcomes: - In-hospital mortality:
- Group 1: 2%
- Group 2: 9.4%
- p = 0.032
- Endotracheal intubation:
- Group 1: 4.1%
- Group 2: 12.5%
- p = 0.04
Discussion
This study demonstrates that early quantification of B-lines via LUS is a powerful predictor of adverse clinical outcomes in AHF. Patients presenting with ≥20 B-lines had significantly higher rates of in-hospital mortality, need for intubation, and persistently elevated NT-proBNP at one year.
These findings support earlier studies in stable HF populations that confirmed the prognostic value of LUS [1,4,9]. In the acute setting, B-line quantification can assist clinicians in identifying high-risk patients who may benefit from intensified decongestive therapy or closer monitoring [3,5].
B-lines reflect extravascular lung water and correlate closely with pulmonary capillary wedge pressure and natriuretic peptides [6,9], making LUS a physiologically relevant, bedside-available tool for real-time patient assessment [8,10].
Limitations
This single-center study maylimitexternal generalizability. Although sonographers followed a standardized scanning protocol, inter-operator variability cannot be excluded. Additionally, echocardiographic parameters such as E/e’ were not included to further validate pulmonary congestion.
Conclusion
Lung ultrasound, particularly B-line assessment, is a valuable tool for early risk stratification in AHF. A B-line count ≥20 on admission is associated with increased in-hospital mortality, higher need for mechanical ventilation, and less favorable biomarker trajectory at 12 months. Integrating LUS into early evaluation protocols may enhance outcome prediction and clinical decision-making in AHF management.
References
- Platz E, Merz AA, Jhund PS, Vazir A, Campbell R, et Dynamic changes and prognostic value of pulmonary congestion by lung ultrasound in acute and chronic heart failure: a systematic review. Eur J Heart Fail 19(9) (2017): 1154–1163
- Pivetta E, Goffi A, Lupia E, Baldassa F, Masellis S, et al. Lung ultrasound-Implemented diagnosis of acute decompensated heart failure in the ED: a SIMEU multicenter Chest 148(1) (2015): 202–210.
- Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein D, Mathis G, et International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38(4) (2012): 577–591
- Platz E, Lewis EF, Uno H, Peck J, Pivetta E, et Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J 37(15) (2016): 1244–1251
- Frassi F, Gargani L, Gligorova S, Ciampi Q, Mottola G, et al. Clinical and echocardiographic determinants of ultrasound lung comets. Eur J Echocardiogr 8(6) (2007): 474–479
- Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, et Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347(3) (2002): 161–167
- Lichtenstein D, Mezière G, Biderman P, Gepner A, Rouby JJ, et al. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Intensive Care Med 24(12) (1998): 1331–1334
- Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound 12 (2014): 25
- Platz E, Pivetta E, Merz AA, Peck J, Rivero J, et al. Prognostic value of pulmonary congestion assessed by lung ultrasound in acute heart failure. Circ Heart Fail 9(11) (2016): e003850.
- Coiro S, Rossignol P, Ambrosio G, Carluccio E, Alunni G, et al. Prognostic value of residual pulmonary congestion at discharge assessed by lung ultrasound imaging in heart failure. Eur J Heart Fail 22(4) (2020): 766–773