Role of Vitamin D Supplementation in the Treatment of Severe Acute Malnutrition
Dr Shibani Datta1*, Prof Dr Mujibul Hoque2, Dr Suman Kanti Chowdhury3, Dr Md. Shohidul Islam Khan4, Dr Purabi Mazumder5, Dr Naima Rahman6
1Registrar, Department of Neonatology, Chittagong Medical College Hospital, Chittagong, Bangladesh
2Professor & Head, Department of Paediatrics, Sylhet MAG Osmani Medical College, Sylhet, Bangladesh
3Assistant Professor, Department of Medicine, Sylhet MAG Osmani Medical College, Sylhet, Bangladesh
4Assistant Professor, Department of Paediatrics, Sylhet MAG Osmani Medical College, Sylhet, Bangladesh
5Resident Physician, 250 Bed District Hospital, Sunamganj, Bangladesh
6Medical Officer (NICU), Government Employee Hospital, Dhaka, Bangladesh
*Corresponding Author: Dr Shibani Datta, Registrar, Department of Neonatology, Chittagong Medical College Hospital, Chittagong, Bangladesh.
Received: 29 July 2025; Accepted: 12 August 2025; Published: 20 August 2025
Article Information
Citation: Shibani Datta, Mujibul Hoque, Suman Kanti Chowdhury, Md. Shohidul Islam Khan, Purabi Mazumder, Naima Rahman. Role of Vitamin D Supplementation in the Treatment of Severe Acute Malnutrition. Journal of Pediatrics, Perinatology and Child Health. 9 (2025): 140-146.
Share at FacebookAbstract
Background: Severe acute malnutrition (SAM) is one of the most common causes of morbidity in children and accounts for 4.4% of deaths worldwide due to severe wasting. It has been found that vitamin D levels are low in children with SAM and in very sick children. The WHO recommendations for the management of SAM include very modest amounts of vitamin D that do not reliably correct deficiency.
Aims of the study: The aims of this study were to determine the effects of vitamin D supplementation on children with severe acute malnutrition.
Methods: This randomized controlled trial was conducted in the Department of Paediatrics, Sylhet MAG Osmani Medical College Hospital, Sylhet, Bangladesh, from January 2021 to December 2022. Seventy two children aged 6 to 59 months with SAM were randomized by lottery method and enrolled as Group A and Group B. Group A received six lakhs IU Vitamin D that was given intramuscularly on admission day along with conventional treatment of SAM, while Group B received only conventional management. Both groups were assessed for weight, height/ length, WHZ/WLZ scores, developmental indexes on admission and after eight weeks of intervention. Cure rate and hospital stay duration were also recorded.
Results: Among the 72 randomly assigned children, 67 participants completed the 8 weeks follow-up and were included in the analysis. Group A exhibited a significantly greater mean weight gain compared to Group B (1.76 ± 0.51 kg vs. 1.26 ± 0.82 kg; p=0.003), which was statistically significant. Although the mean height gain was higher in Group A (0.63 ± 0.59 cm) than in Group B (0.44 ± 0.62 cm), this difference was not statistically significant (p=0.204). Weight-for-height/length Z scores of Group A showed a significantly greater improvement (0.74 ± 1.04 vs. 0.09 ± 1.38; p<0.05) after 8 weeks. Proportion of cured participants (97.2% vs. 88.9%; p=0.16) and the length of hospital stay (8.69 ± 2.99 vs. 10.16 ± 3.78 days; p=0.081) in Group A and Group B were not statistically significant. Neurodevelopmental assessments using Denver Developmental Screening Tool II (DDST-II), revealed lower proportions of delayed gross motor, language and personal/social development in Group A (p<0.05) which were statistically significant. The mean of serum 25(OH)D concentration at the end of study were 77.03 ± 16.64 and 28.88 ± 7.44 ng/ml in Group A and Group B respectively. Serum 25(OH)D concentration exceeded 125 ng/ml in only 1 of 35 participants in Group A without any hypervitaminosis signs.
Conclusion: Vitamin D supplementation in addition to conventional treatment of SAM, significantly enhanced weight gain, improved the mean weight for height/length Z score and developmental indexes in children with uncomplicated severe acute malnutrition.
Keywords
Severe acute malnutrition (SAM); Vitamin D supplementation; WHZ/WLZ; DDST-II; Developmental index; Serum 25-hydroxyvitamin D [25(OH)D]
Severe acute malnutrition (SAM) articles; Vitamin D supplementation articles; WHZ/WLZ articles; DDST-II articles; Developmental index articles; Serum 25-hydroxyvitamin D [25(OH)D] articles.
Article Details
1. Introduction
Severe acute malnutrition (SAM) is the most critical form of undernutrition in children under five and remains a pressing health concern in developing countries like Bangladesh. It is one of the commonest diseases in Bangladesh. SAM contributes significantly to childhood morbidity and mortality, often accompanied by micronutrients and vitamins deficiencies [1]. According to the National Guidelines for the Management of SAM (2017), children aged 6–59 months are classified as having SAM if they have a mid-upper arm circumference (MUAC) <115 mm, a weight-for-height/length Z-score (WHZ/WLZ) <−3 standard deviations (SD) or bilateral pedal edema. For infants under six months, criteria include WLZ <−3SD, visible wasting, or bipedal edema [2]. Globally, approximately 20 million children suffer from SAM, resulting in an estimated one million deaths annually. The majority of this burden occurs in Asia, with more than 12 million affected children across six countries: Afghanistan, Bangladesh, Indonesia, Pakistan, Yemen, and India [3]. In Bangladesh, the prevalence of chronic malnutrition remains high, with nearly 2.4 million children experiencing wasting and approximately 450,000 suffering from SAM [4]. According to the Bangladesh Demographic and Health Survey (BDHS, 2018), 31% of children under five are stunted, 22% are underweight, and 8% are wasted, with Sylhet division exhibiting the highest malnutrition rates [5]. Several risk factors contribute to SAM, including poverty, food insecurity, repeated infections and poor feeding practices, short birth intervals and large family size. The two major clinical forms of SAM are kwashiorkor, caused primarily by protein deficiency and nutritional marasmus, resulting from severe energy deficiency [1]. WHO guidelines for managing SAM recommends therapeutic feeding and routine supplementation with micronutrients such as vitamin A, folic acid, zinc, iron and multivitamin syrup [6]. However, these formulations typically contain limited amounts of vitamin D (≤400 IU), which may not meet the needs of severely malnourished children [7,8]. Vitamin D plays an essential role in immune regulation, inflammatory control, bone development and muscle function [9]. It enhances innate immunity, modulates cytokine production, supports neurological development and facilitates calcium and phosphorus absorption for bone mineralization [10,11]. Children with SAM often have low serum vitamin D levels, which may worsen due to systemic inflammation interfering with vitamin D metabolism [12]. Vitamin D deficiency in these children is associated with impaired immunity, increased infection risk and muscle wasting [13,14]. Few studies have evaluated high-dose vitamin D supplementation in SAM. A study in Pakistan reported improved weight gain and developmental outcomes following administration of two oral doses of 200000 IU vitamin D3 alongside ready-to-use therapeutic food [15]. Another Indian study using 600000 IU intramuscular vitamin D showed improved wasting over two months, though outcome indicators, length of stay in hospital did not differ significantly [12]. The present study was designed to assess the effects of vitamin D supplementation on clinical and developmental outcomes in children suffering from SAM.
2. Methodology and Materials
This study was designed as a randomized controlled trial conducted from 1st January, 2021 to 31st December, 2022 in the Department of Paediatrics at Sylhet MAG Osmani Medical College Hospital, Sylhet, Bangladesh. All children aged 6 to 59 months admitted to the Department of Paediatrics during the study period were screened for severe acute malnutrition (SAM). Children diagnosed with SAM who met the inclusion criteria were enrolled using purposive sampling.
2.1 Inclusion Criteria
- • Children aged between 6 months and 59 months
- • Diagnosed with severe acute malnutrition according to WHO criteria (MUAC<115 mm, weight-for-height/length z-score <-3 SD, or bilateral pedal edema) [16].
2.2 Exclusion Criteria
- • Secondary malnutrition due to underlying chronic illness
- • Clinical evidence of rickets
- • History of vitamin D supplementation within the past six months
2.3 Sample size and Randomization
A total of 72 children meeting eligibility criteria were recruited. They were randomized into two groups by a lottery method through drawing papers from a container: Group A (Vitamin D supplementation with conventional treatment, n=36) and Group B (conventional treatment alone, n=36). During follow-up, 1 child in Group A died due to aspiration pneumonia and 4 children in Group B died from complications including dehydration secondary to gastroenteritis, bronchopneumonia and septicemia. The final analyzed sample comprised 35 children in Group A and 32 children in Group B. Both groups received conventional treatment for SAM based on national protocols. Group A received an additional single dose of intramuscular Vitamin D (600000 IU) after the stabilization phase.
2.4 Data collection procedure
At admission, detailed socio-demographic and clinical histories were obtained from caregivers, including presenting complaints, birth history, socio-economic status, developmental milestones, immunization and feeding practices (exclusive breastfeeding, pre-lacteal feeding and weaning patterns). A thorough physical examination was performed. Anthropometric measurements included weight, height/length, WHZ/WLZ, mid-upper arm circumference (MUAC) and presence of bilateral pedal edema. Weight was measured using a calibrated weighing scale (bathroom scale for standing children; hanging scale for non-ambulatory children) with minimal clothing. Length was measured by an infantometer for infants unable to stand and height by stadiometer for ambulatory children. Weight-for-height/length z-scores (WHZ/WLZ) were calculated according to WHO child growth standards. MUAC was assessed using color-coded MUAC tapes (Shakir’s tape) at the midpoint between the olecranon and acromion processes. Edema was evaluated by applying thumb pressure on the dorsal aspect of both feet for 3 seconds; persistent thumb impression indicated pitting edema [17].
2.5 Developmental assessment
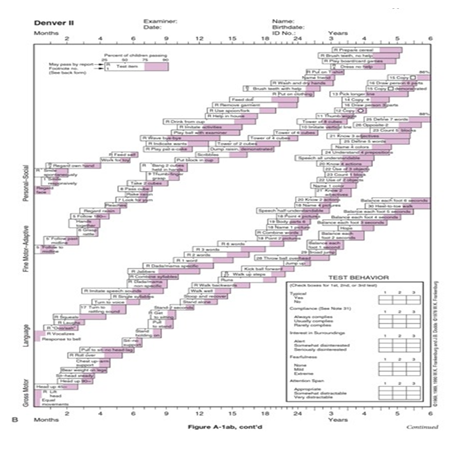
Baseline developmental status was assessed after stabilization using the Denver Developmental Screening Tool II (DDST-II) (Figure 1) [18]. The assessment covered four domains: personal-social, fine motor-adaptive, language and gross motor skills. Tasks appropriate to the child’s age were scored as pass, fail or refused. Using standardized criteria, children were classified as having no delay, caution or delay. Children with ≤1 delay or ≤2 cautions were considered suspicious, while those with ≥2 delays or ≥3 cautions were classified as delayed.
2.6 Follow-up and outcome measures
After stabilization and Vitamin D administration (for Group A), children were followed until discharge, where anthropometry (weight, height/length, WHZ/WLZ), length of hospital stay, cure rate and developmental status were recorded. Further follow-up visits were conducted at 4 and 8 weeks post-discharge. Outcomes measured included clinical improvement (weight gain, height increase, improvement of WHZ/WLZ), developmental progress and serum 25-hydroxyvitamin D [25(OH)D] concentration at the final follow-up.
2.7 Statistical analysis
Data were analyzed using SPSS version 25. Quantitative variables were expressed as mean ± standard deviation and compared between groups using unpaired t-tests. Qualitative variables were presented as proportions and compared using Chi-square tests. A p-value <0.05 was considered statistically significant.
2.8 Ethical considerations
The study protocol was approved by the Ethical Committee of Sylhet MAG Osmani Medical College. Written informed consent was obtained from the parents or legal guardians after explaining the study objectives and procedures. Participants’ confidentiality was strictly maintained and withdrawal from the study was permitted at any time without affecting standard care.
3. Results
A total of 67 participants were included in this study. Table 1 shows, the mean age of participants in Group A was 16.10±11.70 months, while in Group B it was 10.95±7.05 months. Proportion of male was 68.57% and female was 31.43% in Group A, while 65.63% was male and 34.38% was female in Group B. The mean body weight were 6.04 ± 1.71kg and 4.80 ± 1.72 kg, mean height were 66.94 ± 9.40 cm and 61.09 ± 7.42 cm, weight-for-height/length Z score were -2.72 ± 1.19 and -2.79 ± 1.23 and mean MUAC were 112.94 ± 7.95 mm and 108.63±12.82 mm in Group A and Group B respectively on admission. The proportion of participants with delayed global development at were 11.4% and 18.8%, delayed language development were 5.7% and 18.8% and delayed personal or social development were 5.7% and 15.6% in Group A and Group B respectively at baseline. Table 2 illustrates changes in weight and height over 8 weeks. Weight increased from baseline to 8 weeks, 7.80±1.79 kg in Group A and 6.09±1.98 kg in Group B, with a weight gain of 1.76±0.51 kg and 1.26±0.82 kg, respectively. The comparison of mean of weight gain was significantly higher in Group A (p<0.05). Height increased to 67.57±9.33 cm and 61.53±7.40 cm in Group A and Group B, with a height gain of 0.63±0.59 cm and 0.44±0.62 cm, respectively; which was not statistically significant (p0.05). Table 3 shows, the mean weight for height/length Z score in Group A and Group B were -2.72±1.19 and -2.79±1.23 respectively on admission and 0.74±1.04 and 0.090±1.38 at 8 weeks respectively. The mean weight for height/length Z score was statistically significant (p0.05) in Group A after 8 weeks. Table 4 shows, there was no significant (p value>0.05) association between Vitamin D supplementation and outcome indicators such as ‘cured’ and ‘death’ between the two groups. The average hospital stay was 8.69±2.99 days in Group A and 10.16±3.78 days in Group B respectively that was not statistically significant (p0.05). Developmental outcomes after 8 weeks are displayed in Table 5. Proportion of participants having delayed gross motor development were 8.6% in Group A and 28.1% in Group B, language development delays were recorded in 0% of Group A and 12.5% of Group B, personal-social development delays were found in 0% of Group A and 12.5% of Group B respectively at 8 weeks of follow up. Comparison of these were statistically significant (p0.05) between two groups. Proportion with delayed global development were 8.6% in Group A and 15.6% in Group B and delayed fine motor development was 5.7% in Group A and 18.8% in Group B at 8 weeks, those were statistically not significant (p0.05). Table 6 shows, after 8 weeks, the mean of Serum 25(OH)D concentration was 77.03±16.64 ng/ml in Group A and 28.88 ± 7.44 ng/ml in Group B (p<0.001).
|
Characteristics |
Group A (n = 35) |
Group B (n = 32) |
|
Age (months), mean ± SD |
16.10 ± 11.70 |
10.95 ± 7.05 |
|
Gender, n (%) |
||
|
Male |
24 (68.57) |
21 (65.63) |
|
Female |
11 (31.43) |
11 (34.38) |
|
Anthropometry (mean ± SD) |
||
|
Weight (kg) |
6.04 ± 1.71 |
4.80 ± 1.72 |
|
Height (cm) |
66.94 ± 9.40 |
61.09 ± 7.42 |
|
Weight-for-length/height Z-score (WLZ/WHZ) |
-2.72 ± 1.19 |
-2.79 ± 1.23 |
|
Mid-upper arm circumference (MUAC, mm) |
112.94 ± 7.95 |
108.63 ± 12.82 |
|
Proportion of participants with delayed developmental status, n/total n (%) |
||
|
Global Development |
5 (14.29) |
6 (18.75) |
|
Gross Motor Development |
5 (14.29) |
9 (28.13) |
|
Fine Motor Development |
4 (11.43) |
6 (18.75) |
|
Language Development |
2 (5.71) |
6 (18.75) |
|
Personal-Social Development |
2 (5.71) |
5 (15.63) |
Table 1: Baseline demographic, anthropometric and developmental characteristics of the study population.
|
Parameter |
Group A |
Group B |
p-value |
|
Weight (kg) |
|||
|
Admission |
6.04 ± 1.71 |
4.83 ± 1.72 |
0.003 |
|
After 8 weeks |
7.80 ± 1.79 |
6.09 ± 1.98 |
|
|
Weight Gain |
1.76 ± 0.51 |
1.26 ± 0.82 |
|
|
Height (cm) |
|||
|
Admission |
66.94 ± 9.41 |
61.09 ± 7.42 |
0.204 |
|
After 8 weeks |
67.57 ± 9.33 |
61.53 ± 7.40 |
|
|
Height Gain |
0.63 ± 0.59 |
0.44 ± 0.62 |
|
Table 2: Comparison of changes in body weight and height from baseline to 8 weeks following treatment in the study population.
|
WHZ / WLZ |
Group A |
Group B |
p value |
|
Admission |
-2.72±1.19 |
-2.79±1.23 |
0.827 |
|
After 8 weeks |
0.74±1.04 |
0.09±1.38 |
0.032 |
Table 3: Weight for Height/Length Z score at Admission and after 8 Weeks.
|
Outcome |
Group A |
Group B |
p-value |
|
Cured, n (%) |
35 (97.22) |
32(88.9) |
0.16 |
|
Death, n (%) |
1 (2.78) |
4 (11.11) |
|
|
Length of hospital stay (days) |
8.69 ± 2.99 |
10.16 ± 3.78 |
0.081 |
|
(Mean ± SD) |
Table 4: Clinical outcomes: cure rate, mortality and Length of hospital stay.
|
Proportion of participants with delayed developmental outcomes |
Group A n/total n (%) |
Group B n/total n (%) |
p value |
|
Global Development |
3(8.6%) |
5(15.6%) |
0.374 |
|
Gross Motor Development |
3(8.6%) |
9(28.1%) |
0.037 |
|
Fine Motor Development |
2(5.7%) |
6(18.8%) |
0.101 |
|
Language Development |
0(0.0%) |
4(12.5%) |
0.031 |
|
Personal-Social Development |
0(0.0%) |
4(12.5%) |
0.031 |
Table 5: Developmental outcomes at 8 weeks post-treatment in the study population.
|
Parameter |
Group A |
Group B |
p-value |
|
Serum 25(OH)D concentration (ng/ml) |
77.03 ± 16.64 |
28.88 ± 7.44 |
<0.001 |
Table 6: Serum Vitamin D levels of Group A and Group B at 8 weeks.
4. Discussion
Severe acute malnutrition remains a critical public health challenge worldwide, especially in low and middle income countries, where it significantly increases under-five morbidity and mortality. While Vitamin D is well-established for its role in bone metabolism, emerging evidence highlights its immunomodulatory and anti-inflammatory properties, which may influence recovery in malnourished children [19]. However, only few randomized controlled trials has been conducted to investigate the effects of Vitamin D supplementation in children with SAM. The current study was conducted to assess the role of vitamin D supplementation as an adjunct to conventional nutritional therapy in children with SAM. A total of 72 children were assessed for eligibility; among them 36 were allocated to Group A (Vitamin D plus conventional treatment) and 36 to Group B (conventional treatment only). One child in Group A and four in Group B died; the remaining participants completed the follow-up and were included in the analysis. In the present study, the mean age of participants was 13.5 months (range: 6–59 months), with females comprising 32.8% (22/67). The mean weight and height of total participants were 5.4 kg (range: 2.5–10 kg) and 64.01 cm (range: 49–96 cm) respectively. Mean weight-for-height/length Z score was –2.8 (range: –5.6 to –1.0) and mean mid-upper arm circumference (MUAC) was 110.79 mm (range: 70–130 mm). The proportion of participants with delayed global development was found 16.56%; while gross motor, fine motor, language and personal-social delays were noted as 21.20%, 15.10%, 12.25% and 10.65%, respectively at baseline (Table 1). The mean of weight gain from baseline to 8 weeks were 1.76 ± 0.51 kg and 1.26 ± 0.82 kg in Group A and Group B respectively (Table 2), which was statistically significant (p=0.003) between two Groups. Saleem et al. [15] reported that high-dose Vitamin D supplementation in addition to conventional treatment significantly improved weight gain, aligning with our findings [15]. However, Maurya et al. [12] observed no significant difference, possibly due to their use of average weight gain in gm/kg/day instead of mean weight gain, which may explain the discrepancy in results [12]. In the present study, the mean height gain at 8 weeks were 0.63±0.59cm in Group A and 0.44±0.62cm in Group B (Table 2), with no statistically significant difference (p=0.204). This finding is consistent with that of Maurya et al. [12], who also reported no significant improvement in height following Vitamin D supplementation [12]. Saleem et al. [15] did not assess height gain between two groups [15]. However, the mean weight-for-height/length Z score at 8 weeks was significantly higher in Group A (0.74±1.04) compared to Group B (0.090±1.38) (p=0.032) (Table 3), aligning with findings by Maurya et al. [12] and Saleem et al. [15]. The proportion of cured patients were 97.2% in Group A and 88.9% in Group B, with deaths of 2.8% and 11.1%, respectively (Table 4). No significant association was observed between Vitamin D supplementation and outcomes (p=0.16), consistent with Maurya et al. [12]. The length of hospital stay in Group A and Group B were 8.69±2.99 days and 10.16±3.78 days respectively (Table 4) that was not statistically significant (p=0.081). Maurya et al (2018) also found that Vitamin D supplementation does not have any significant improvement in average length of stay in hospital. So the result is in well agreement with the current study. Similarly, other studies have found no significant effect of vitamin D on hospital stay length, although some suggest potential benefits in specific subgroups [20]. Analysis of individual components of the Denver Development Screening Tool II (DDST II) (Figure 1) in the present study demonstrated (Table 5) that Vitamin D supplementation significantly reduced delays in gross motor development (p=0.037), language development (p=0.031) and personal-social development (p=0.037) after 8 weeks of follow-up. However, no statistically significant improvements were observed for fine motor development (p=0.101) and global development (p=0.036). Contrarily, Saleem et al. [15] reported that high-dose Vitamin D3 significantly improved global, gross motor, fine motor and language development, but not personal-social development at 8 weeks. The discrepancies between these findings may stem from differences in therapeutic protocols, notably the use of F75 formula in the current study versus Ready-to-Use Therapeutic Food (RUTF) employed in the Pakistani study, which may influence recovery and developmental outcomes in severe acute malnutrition. In biochemical analyses, the mean serum 25(OH)D concentration at study completion were 77.03 ± 16.64 ng/ml and 28.88 ± 7.44 ng/ml in Group A and Group B respectively (p<0.001) (Table 6). Only 2.86% of Group A exceeded 125 ng/ml without hypervitaminosis symptoms. Similar findings were reported by Saleem et al. [15].
Limitations of the study: Every hospital-based study has some limitations and the present study undertaken is no exception to this fact. The limitations of the present study are mentioned.
- • The sample size of the study was small.
- • The study was carried out in single center.
- • The study did not conduct a dose response study as it remains unclear whether a lower dose would be sufficient to boost weight gain to a similar extent.
5. Conclusion and Recommendations
This study concluded that administration of Vitamin D in addition to conventional treatment of SAM significantly enhanced weight gain, mean weight for height/length Z score and gross motor development, language development and personal or social developmental status at the 8 weeks of follow up in children with severe acute malnutrition. Therefore, vitamin D administration favorably impacts key developmental domains, suggesting benefits beyond mere nutritional rehabilitation. Given the high burden of developmental delays and poor growth in this population, integrating vitamin D supplementation into SAM management protocols could enhance recovery and long-term child health outcomes. Further large-scale, randomized controlled trials are warranted to confirm these findings and to establish optimal dosing regimens.
Funding: No funding sources.
Conflict of interest: None declared.
Ethical approval: The study was approved by the Institutional Ethics Committee.
References
- Gupte S. The Short Textbook of Pediatrics. JP Medical Ltd (2016).
- Fahim SM, Islam MR, Rasul MG, et al. A qualitative assessment of facility readiness and barriers to the facility-based management of childhood severe acute malnutrition in the public healthcare settings in Bangladesh. Public Health Nutrition 25 (2022): 2971-82.
- Ahmed T, Hossain M, Mahfuz M, et al. Severe acute malnutrition in Asia. Food and Nutrition Bulletin 35 (2014): S14-26.
- Rahman M. Assessment of Nutritional Status of Primary School Going Children in Island and Hill-Tract Area of Bangladesh: A Cross-Sectional Study (Doctoral dissertation, Chittagong Veterinary and Animal Sciences University Chittagong–4225, Bangladesh).
- Sanin KI, Khanam M, Rita RS, et al. Common factors influencing childhood undernutrition and their comparison between Sylhet, the most vulnerable region, and other parts of Bangladesh: Evidence from BDHS 2007–18 rounds. Frontiers in Nutrition 9 (2023): 999520.
- Vir SC. Iron Deficiency Anaemia: Anaemia Prevention and Control Programme: Evolvement of Policies and Programme, 1970–2017 and Anaemia Mukt Bharat (AMB) 2018. In Child, Adolescent and Woman Nutrition in India 13 (2023): 248-310.
- Moon RJ, Curtis EM, Cooper C, et al. Vitamin D supplementation: are multivitamins sufficient?. Archives of disease in childhood 105 (2020): 791-3.
- Merker M, Amsler A, Pereira R, et al. Vitamin D deficiency is highly prevalent in malnourished inpatients and associated with higher mortality: A prospective cohort study. Medicine 98 (2019): e18113.
- Berkley JA, Ngari M, Thitiri J, et al. Daily co-trimoxazole prophylaxis to prevent mortality in children with complicated severe acute malnutrition: a multicentre, double-blind, randomised placebo-controlled trial. The Lancet Global Health 4 (2016): e464-73.
- Eyles DW, Feron F, Cui X, et al. Developmental vitamin D deficiency causes abnormal brain development. Psychoneuroendocrinology 34 (2009): S247-57.
- Hazell TJ, DeGuire JR, Weiler HA. Vitamin D: an overview of its role in skeletal muscle physiology in children and adolescents. Nutrition Reviews 70 (2012): 520-33.
- Maurya M, Sharma P, Srivastava A, et al. Effect of vitamin D supplementation in children with severe acute malnutrition in a nutritional rehabilitation centre: a randomized controlled trial. Pediatr Rev Int J Pediatr Res 5 (2018): 278-83.
- Song C, Sun H, Wang B, et al. Association between vitamin D status and undernutrition indices in children: a systematic review and meta-analysis of observational studies. Frontiers in Pediatrics 9 (2021): 665749.
- Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ 15 (2017): 356.
- Saleem J, Zakar R, Zakar MZ, et al. High-dose vitamin D3 in the treatment of severe acute malnutrition: a multicenter double-blind randomized controlled trial. The American Journal of Clinical Nutrition 107 (2018): 725-33.
- Grellety E, Golden MH. Severely malnourished children with a low weight-for-height have similar mortality to those with a low mid-upper-arm-circumference: II. Systematic Literature Review and Meta-Analysis. Nutrition journal 17 (2018): 80.
- Multicentre Growth Reference Study Group, de Onis M. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatrica 95 (2006): 76-85.
- Ryu SH, Sim YJ. The validity and reliability of DDST II and Bayley III in children with language development delay. Neurology Asia 24 (2019): 355-61.
- Ibrahim MK, Zambruni M, Melby CL, et al. Impact of childhood malnutrition on host defense and infection. Clinical microbiology reviews 30 (2017): 919-71.
- Amrein K, Schnedl C, Holl A, et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA 312 (2014): 1520-30.