Systemic Health Intervention Design through Participatory Modeling: Low-dose Aspirin for Women at Risk of Preeclampsia
Yin Jien Lee*,1, Leslie Kowalewski1,2, Jeff Gould1,3, Lindsay du Plessis1,2, Bryan Oshiro4, Melody Moua5, David K Stevenson1,2, Gary L Darmstadt1
1Department of Pediatrics, Stanford University School of Medicine, Stanford, California, USA
2California Maternal Quality Care Collaborative (CMQCC), Stanford University School of Medicine, Stanford, California, USA
3California Perinatal Quality Care Collaborative (CPQCC), Stanford University School of Medicine, Stanford, California, USA
4Riverside University Health System (RUHS), Riverside, California, USA
5School of Humanities and Sciences, Stanford University, California, USA
*Corresponding author: Yin Jien Lee, Department of Pediatrics, Stanford University School of Medicine, Stanford, California, USA
Received: 18 July 2025; Accepted: 28 July 2025; Published: 20 August 2025
Article Information
Citation: Yin Jien Lee, Leslie Kowalewski, Jeff Gould, Lindsay du Plessis, Bryan Oshiro, Melody Moua, David K Stevenson, Gary L Darmstadt. Systemic Health Intervention Design through Participatory Modeling: Low-dose Aspirin for Women at Risk of Preeclampsia. Fortune Journal of Health Sciences. 8 (2025): 798-813.
Share at FacebookAbstract
Preeclampsia (PE) and eclampsia accounted for 7% of maternal mortality in the United States (2016 – 2018). In California, in-hospital diagnosed PE rates rose from 4.6% to 8.1% (2017-2023), with severe cases increasing from 2% to 4% and mild-to-moderate cases from 1% to 2.7%. Clinical guidelines recommend a daily low-dose aspirin (LDA) regimen of 81 mg starting at 12 weeks’ gestation for at-risk women. However, uptake rates remain suboptimal (47% to 79%). Informed by the literature, women with lived experiences for complicated pregnancies, and healthcare stakeholders in Riverside, California, we developed a participatory system dynamics (SD) simulation model, incorporating focus groups, group model building (GMB), and simulation modeling to identify interventions that could increase LDA uptake. The simulation tested 26 scenarios. Six key drivers of increased LDA uptake were identified: (1) frequency of women’s interpersonal contacts, (2) dissemination of information by authoritative organizations online, (3) time required for nurse training on LDA protocols, (4) timing of enrollment in home visiting programs, (5) capacity of trained home visitors, and (6) awareness of home visiting programs among pregnant women. Optimizing these variables increases projected LDA uptake by 63% over 120 months. Our findings demonstrate how participatory modeling can identify actionable system-level interventions to improve guideline adherence and maternal health.
Keywords
system dynamics, systemic intervention, low-dose aspirin, group model building, participatory modeling, preeclampsia, model optimization
system dynamics articles, systemic intervention articles, low-dose aspirin articles, group model building articles, participatory modeling articles, preeclampsia articles, model optimization articles.
Article Details
Introduction
Preeclampsia (PE) is a hypertensive disorder affecting 4% of pregnancies in the United States. [1]. PE accounted for 7% of maternal mortality between 2016 and 2018 [2, 3]. In California, in-hospital diagnosed PE rates rose from 4.6% to 8.1% between 2017 and 2023 [4, 5]. PE is associated with early labor induction, cesarean delivery, preterm birth, neonatal seizures, and mortality [6]. Women with a history of PE, in vitro fertilization, multifetal gestation, chronic hypertension, diabetes, kidney disease, age over 35, or African American ethnicity are at increased risk [7]. Daily low-dose aspirin (LDA, 81 mg) starting at 12 weeks of gestation for at-risk women is recommended [8].However, despite robust clinical guidance, the uptake of LDA remains low or inconsistent [9-14] (Appendix 1).
Medication decision-making during pregnancy is influenced by women’s risk perception, experiences, values, and beliefs, quality and timeliness of provider communication, social networks, and access to medication and care [15-17]. Many women expressed concern that medication use could cause birth defects, miscarriage, or allergic conditions in their child. Aspirin, a nonsteroidal anti-inflammatory drug (NSAID), is often viewed as particularly risky. And women tended to overestimate the risk of using medicines during pregnancy [18]. These factors interact across individual, clinical, and system levels, making single-point interventions ineffective. We applied a systemic intervention design using system dynamics (SD) modeling and participatory methods to identify key intervention points to improve LDA uptake among at-risk women.
Methods
Study design
To address the wicked problem of medication decision-making involving multiple bidirectional interacting variables, we applied a systemic intervention design to integrate multiple methods from different paradigmatic perspectives, using a SD approach to define problem boundaries [19] and synthesize knowledge. SD is a simulation and mathematical modeling methodology used to understand complex systems and improve decision-making by capturing feedback, delays, and nonlinear behaviors over time [20]. A SD model represents real-world systems through interrelated feedback loops composed of stocks, flows, auxiliaries, and constants. The modeling process follows four iterative stages: conceptualization, formulation, testing, and implementation [21].
The selection of methods in our study was based on synergies across methods arranged in sequence. We began with a literature review to construct a causal map (Appendix 2) that defined the model boundary, identifying key system components, and their interactions, which influence at-risk women’s decisions to initiate and adhere to LDA treatment, forming a preliminary theory to explain how these factors are related [22]. Next, we developed a conceptual SD simulation model to test hypotheses about the decision-making process, and in the process, we identified gaps where the literature lacked sufficient evidence to support specific connections, highlighting areas requiring further investigation. Because not all the necessary information required to run the model was available from the literature, certain assumptions were incorporated into the model. To validate and refine these assumptions, we listed 28 guiding questions for use in the focus group study and group model building (GMB) workshop (Table 1). We then conducted focus groups with women who had experienced pregnancy-related medication challenges to refine and validate the model boundary. In addition, we conducted GMB sessions to gain the insights of multiple stakeholders. Subsequently, we performed model optimization to identify potential systemic intervention points and the best combination of parametric values for selected variables most likely to lead to the highest LDA uptake. All participants in focus group and GMB sessions were administered informed consent, and sessions were audio- and video-recorded and saved in an encrypted cloud drive stored on the university’s server.
Table 1: Guiding Questions Used in the Focus Group Discussion and Group Model Building Workshops
|
Patient-factors |
|
|
1 |
Will more information about the safety of aspirin increase or reduce concern about its safety? |
|
2 |
Will more treatment choices encourage patients to take up or adhere to aspirin? |
|
3 |
Will patients be more likely to take up and adhere to aspirin if the perceived quality of care is high? |
|
4 |
Are pill burden and time to take aspirin relevant in low-dose aspirin (LDA) intervention? |
|
5 |
Will the increase in providers' knowledge of LDA treatment increase the quality of recommendations? Either in the medication routine or other aspects? |
|
6 |
Are patients facing pregnancy complications more prone to developing depression? |
|
7 |
When patients feel that they have more control over their situation or in managing their complications, will they be less likely to be anxious or depressed? More motivated to participate in treatment? |
|
8 |
Do patients who are more willing to manage their health believe they have more resources for their treatment? |
|
9 |
Does patients' motivation increase their self-efficacy? |
|
10 |
Will more effective communication with patients lead to higher quality of communication from providers? How? |
|
11 |
What happens if the physicians try to convince you to take aspirin? |
|
12 |
How long does it take you to consider and adopt physicians' recommendations? |
|
Provider-factors |
|
|
1 |
What are the roles of knowledge in aspirin treatment in physicians' communication with patients? |
|
2 |
How do physicians use the knowledge? |
|
3 |
How do patients receive recommendations? |
|
4 |
What are physicians' efforts in conveying this knowledge to patients? |
|
5 |
When is the ideal time to convey this knowledge and recommendation to patients? |
|
6 |
Do patients' desire for autonomy affect the interactions? |
|
7 |
What if there are no treatment choices? |
|
8 |
Will the increase in providers' knowledge of LDA treatment increase the quality of recommendations? Either in the medication routine or other aspects? |
|
9 |
When patients fail to perform what the providers expect, will the providers put in extra effort to convince the patients? Or divert attention to more engaged patients? |
|
10 |
Are patients facing pregnancy complications more prone to developing depression? (From providers’ perspective) |
|
11 |
Will more effective communication with patients lead to higher quality of communication from providers? How? |
|
System-level Factors |
|
|
1 |
Do the opinions of spouses, family members, and friends form the normative beliefs of patients? |
|
2 |
When patients need more information quickly, do they go to the providers or community? |
|
3 |
Does information from non-profit organizations play a major role in feeding information to patients? |
|
4 |
Aspirin dispensary issues |
|
5 |
What are the roles of local policy in promoting Aspirin intervention at the community level? |
Focus Group Study
We conducted a focus group study to validate and refine the model's assumptions, focusing on the questions outlined in Table 1. The lived experiences and perspectives of these women provided valuable insights into these questions. A focus group study relies on group processes to explore and clarify each other’s views on open-ended questions [23]. We encouraged the participants to explore issues important to them in their own words, express cultural values and group norms, and identify their own questions and priorities. This process supported the expansion and refinement of the model boundary.
Participants, Study Design, and Procedure
Five women known to the California Maternal Quality Care Collaborative (CMQCC) Patient Advisory Committee (PAC) were invited to participate in the study. The CMQCC PAC is composed of individuals with lived experience of PE or other adverse pregnancy outcomes at CMQCC pilot hospitals across California. Participant responses were recorded and categorized into two primary themes: internal and external factors. Internal factors refer to personal beliefs, emotions, or perceptions that participants identified as influencing their decisions to take or avoid medications during pregnancy, including LDA. External factors encompass influences originating outside individuals, such as healthcare provider communication, social support, or access to care. Previous studies estimated that saturation of information—the point at which the linking concepts of two consecutive discussions no longer yield new themes or codes—can typically be achieved after three to six sessions within a homogeneous group using a semi-structured discussion format [24, 25]. Over 60% of the new themes often emerge after the first group discussion, increasing to 84% after the second and third discussions combined. By the sixth session, over 90% of themes are typically identified [24, 25]. Five one hour-long online semi-structured focus group sessions were conducted between January and March 2024. Participants were asked three to four questions from the Patient- and System-level factors in Table 1. One researcher guided the discussion, and the assisting researcher took notes. The first session began with a brief introduction of the project, outlining the session structure and explaining expectations for the focus group. In subsequent sessions, the facilitator began by recapitulating the previous discussion and then introduced new guiding questions for the session.
Data Coding
Coding facilitates the organization of data and thematic integration, allowing qualitative data to be analyzed, assembled, categorized, and sorted to construct meaning [26]. We employed a three-phase coding process based on Grounded Theory, which consists of open coding, axial coding, and selective coding —a systematic qualitative inquiry approach that enables researchers to codify and categorize data, construct theories, and conduct comparative analyses [27]. During the open coding phase, data are broadly examined to identify preliminary themes and establish initial thematic domains. These themes are further refined and connected in the axial coding phase, focusing on relationships between categories and subcategories. In the selective coding phase, themes are integrated selectively to produce cohesive meanings to promote theory development. Because we had established foundational thematic domains from the causal map constructed with information grounded in literature, we were able to bypass the open coding phase and proceed directly to axial and selective coding.
Group model building
GMB is a participatory model building activity which relies on a system-based, collaborative, and facilitated process to engage stakeholders in a group setting to elicit their views of a problem, build common language, and achieve consensus to define and investigate a problem [28, 29]. Engaging stakeholders from problem definition to solution design can potentially increase stakeholders’ buy-in, build alliances, and gain support during the implementation stage [30].
Background of participants and GMB Process
Recruitment flyers were emailed to healthcare providers within Riverside University Health System (RUHS) and to community-based providers. Over a two-month recruitment period, we successfully enrolled a total of eight healthcare providers [an obstetrician-gynecologists(OB-GYNs), a family medicine physician, a pharmacist, a nurse, two doulas, a representatives of community clinics, and a representative of county health department’s home visiting programs]. To accommodate the participants' working schedules, each session was offered twice—once in the afternoon and once in the evening. A total of 12 one-hour virtual GMB workshops were conducted during January-March 2025, along with one in-person session at RUHS. The facilitation team consisted of a lead researcher and a first-year occupational therapy student. During the first two sessions, the team introduced the project objectives, outlined the GMB methodology, explained basic systems thinking concepts, and presented simplified structures of the simulation model. In each subsequent session, a relevant model structure was introduced, and participants were guided through a series of questions focusing on provider-related factors, as outlined in Table 1. In the last in-person workshop, we presented and validated the causal loop diagrams and partial stock-and-flow diagrams with the participants. Then, we shared our model-based analysis with the participants.
Riverside, California
Riverside County, with a population of 2.4 million in 2020 [31],is located in thesouthern portionof theU.S. stateofCalifornia and is 60 miles east of Los Angeles. The median age was 37 years. Hispanics comprise 54.9% of the population, followed by Whites (32.6%), Asians (6.8%), Blacks (6.0%), and others (1.3%). The gender distribution was nearly equal, with a slight female majority (0.4%). Approximately 7.9% of residents were uninsured. In 2023, 6.7% of the county’s population (507,866 persons) consisted of women of reproductive age [32]. Between 2021 and 2023, 13.1% of women (10,325) had pregnancy-associated hypertension at deliveries [32]. While this condition affected fewer than 20% of women in each age group, the prevalence among Black women was nearly 50% higher than that of other racial and ethnic groups. From 2018 to 2022, 43 maternal deaths occurred in Riverside County during pregnancy or within 42 days postpartum due to pregnancy-related causes. Of these, 20 deaths were directly attributed to pregnancy-related conditions [33].
System Dynamics Modeling and Simulation
Based on literature review, focus groups, and GMB, we used Stella Architect to formulate a preliminary SD model to represent the structural and behavioral dynamics of women’s decision-making around LDA uptake. Parameters were initialized within reasonable bounds. For example, the contact rate was set at 3, indicating that each woman communicates with three others about PE or LDA. The initial ratio of correct community information was set to 0.528, a parametric value calculated by Stella Architect to reflect equilibrium—where stock inflows equal outflows [34]. When the model is in equilibrium, we can identify conditions needed to maintain and disrupt the steady state. We validated the model with direct structure tests first, followed by the structure-oriented behavior tests to determine its robustness and build confidence in the model [35]. Structural validity tests assessed how accurately the model represents real-world systems, while behavioral validity tests examined the model’s outcomes under different conditions. Following validation, we conducted scenario analyses to identify interventions that significantly increased LDA uptake and women’s knowledge, which were defined as the “payoffs” in the optimization process. Optimization in SD refers to the act of maximizing or minimizing parametric values of the model against one or a set of criteria in order to improve the model's performance through simulation [36]. Using the Differential Evolution (DE) algorithm in Stella Architect, we identified optimal values for the most influential variables. DE is well-suited for non-linear, multi-dimensional problems due to its efficiency, scalability, and ability to locate global optima [37]. We tested multiple scenarios, altering one or more variables while holding others constant, to evaluate the combined impact of potential interventions [38].
Results
Model Refinement Process
Model v1 - A Generic Model Grounded in Literature
Analysis of the interrelationships among variables derived from the literature review revealed multilateral connections, expanding the model’s complexity (Figure 1). This evidence formed the foundation for the initial version of the model (v1), which comprises four interconnected modules: (1) Patient/Pregnant Women Logistics, (2) Providers, (3) Pregnant Women’s Decision-Making Process, and (4) System-Level Factors.
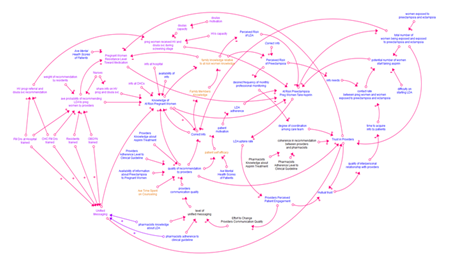
Figure 1: Causal Loop Diagram Exhibiting Progressive Changes from Literature Review to Focus Group Discussion and Group Model Building
Note: Blue – structure built with information from the literature; orange – structure built after focus groups; purple – structure built after GMB; black – structure removed after GMB.
Patient/Pregnant Women Logistics Module
The Patient or Pregnant Women Logistics module serves as the core component of the model (Figure 2). It tracks women from entry into reproductive age through their first pregnancy. Women exit the model upon entering a second pregnancy, death, or discontinuing LDA for more than 60 days. To focus on the women’s decision-making process, the model emphasizes the first pregnancy journey of at-risk women. Early in pregnancy, women are screened for PE risk. Those identified as at risk receive LDA counseling and may either initiate and adhere to the treatment throughout pregnancy or discontinue it. If nonadherence is identified within 30 days—typically during a clinical visit—providers may re-engage the patients to the treatment. Otherwise, resistance to treatment increases, making reinitiation unlikely. Women not identified as at risk proceed through pregnancy without LDA, though some may still develop eclampsia.
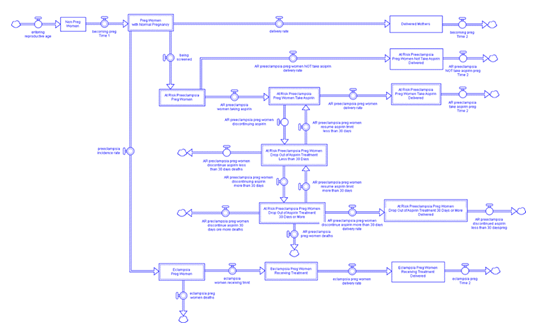
Figure 2: Simplified Stock and Flow Structure in the Patient/Pregnant Women Logistics Module of the System Dynamics Simulation Model
Providers Module
The providers module comprises interacting factors related to providers’ communication quality, adherence to guidelines, the information available to their patients, their perception of patients’ engagement with their recommendations, and their efforts to improve their communication with patients (Appendices 3a & 3b). Providers’ knowledge, adherence to clinical guidelines, information provided to women, and communication quality all positively influence the quality of providers' recommendations. On the other hand, providers’ perception of patients' engagement affects providers’ effort to improve their communication style. As providers improve their communication quality and pharmacists enhance their knowledge about LDA treatment and adhere to the clinical guidelines, the messaging to women becomes more unified. A unified messaging helps improve providers' communication quality.
Pregnant Women Decision-making Process Module
This complex module outlines the causal mechanisms influencing women’s decisions regarding LDA uptake (Appendices 4a and 4b). Women’s perceptions of PE and LDA risks are shaped by their knowledge, directly impacting their decisions. Higher perceived risk of PE is associated with a greater desire for frequent monitoring, which, when paired with coordinated care, consistent messaging from pharmacists and providers, and high-quality recommendations, strengthens trust in providers. This mutual trust enhances provider–patient relationships, thereby improving information exchange. The closer the relationship, the easier it is for women to receive the information they need from their providers. Adherence to LDA is also influenced by the quality of provider recommendations, which is positively linked to women's self-efficacy. Confidence in managing medication motivates women to stay on treatment. However, PE screening may heighten anxiety [39, 40], which can negatively affect self-efficacy [41].
System-level Factors Module
This module illustrates how information is disseminated among women with prior experience of LDA use, eclampsia, or preterm birth, those currently at risk, and at-risk women and their families (Appendix 5a). The ratio of correct to incorrect information fluctuates based on community exchanges and content from authoritative online sources. Only correct information contributes positively to women’s knowledge. A higher perceived risk of PE, shaped by effective provider communication and accurate community information, motivates women to seek further guidance through peer discussions (Appendix 5b). As positive experiences and accurate information spread, LDA uptake among at-risk women increases.
Model v2 – Model Refined with Focus Group Study Data
This version was refined using insights gathered from focus groups. From these discussions, we identified 22 main themes matching the variables in the causal map and 26 new sub-themes through axial coding and the relationships between the themes and sub-themes (Appendix 6). Notably, several participant insights revealed discrepancies between our initial assumptions, based on literature-derived data, and the lived experiences shared during the discussions.
Insight 1 – Family Members' Opinions are Influential in Pregnant Women's Medication Decisions
Participants emphasized the significant influence of family members on their decision-making. While they expressed trust in healthcare providers’ recommendations, they often sought additional input from family, valuing the different perspectives offered. Compared to broader community information, family support held greater weight. The Family Members' Knowledge is shaped by the accuracy of information circulating within the community (Figure 1). When discrepancies arise between the knowledge held by women and their family members, participants reported prioritizing their family’s opinions. In cases where family members possessed limited or inaccurate information, this tended to diminish the perceived risk of PE.
Insight 2 – Patients' self-efficacy affects motivation
Previous assumptions suggested that patients’ motivation influenced both self-efficacy and mental health, which in turn reinforced motivation (Figure 1). Focus group participants expressed that while receiving providers' recommendations was stressful, stress did not lead to depression or diminish motivation. Instead, self-efficacy emerged as a key driver of medication uptake. Participants noted that patients with greater resources and support were more likely to initiate and adhere to treatment. One participant emphasized that patients actively secured these resources by seeking information and engaging with providers, which enhanced their readiness for treatment. Increased provider interaction also fostered trust, further contributing to higher aspirin uptake.
Insight 3 – Time spent on counseling patients
Previously, the quality of provider recommendations in the model was influenced by two factors: Providers’ Knowledge of Aspirin Treatment and Adherence to Clinical Guidelines (Figure 1). However, participants emphasized the importance of the time that providers spent explaining PE risks and LDA benefits. As a result, Average Time Spent on Counseling was added as a third factor influencing recommendation quality.
Insight 4 – Uncertain relationship between patients’ mental health, motivation, and self-efficacy
The perceived helplessness in controlling the outcome of a disease might lead to loneliness and depression [41]. However, the participants highlighted that a lack of self-efficacy would not affect their mental health. Contrarily, they would seek more information to increase their self-efficacy in addressing pregnancy complications.
Model v3 – Model Refined with Focus Group Study and Group Model Building Data
Model v3 was revised based on insights from GMB workshop participants, incorporating six new modules (Figure 3): RUHS Provider Capacity and Training, Information Availability, Community Provider Home Visiting and Doulas, Pharmacist Training, Recommendation and Referral Process, and Unified Messaging.
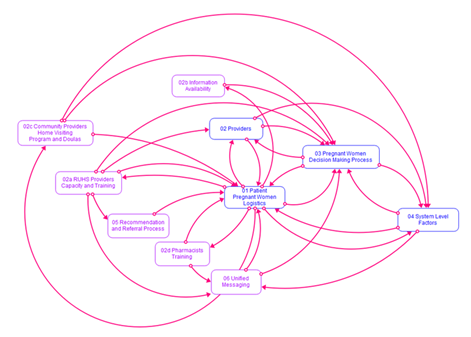
Figure 3: Model Version 3 - The Original and New Module Resulting from Group Model Building Workshops
Note: Blue boxes represent the modules in Model v1 and v2. The purple boxes are newly added modules after GMB workshops.
RUHS Provider’s Capacity and Training Module
This module illustrates the capacity and training of family medicine physicians, faculty, residents, OB-GYNs, nurses, and community clinic providers (Appendix 7). Trained family medicine doctors screen and counsel at-risk patients during routine visits, documenting these discussions in patient charts for OB-GYNs to review at subsequent prenatal appointments. Family physicians also train residents in PE screening and LDA counseling; however, residents may defer to mentors when encountering patient resistance. Generally, OB-GYNs are trained in PE screening and LDA treatment, but their counseling practices vary based on personal perceptions of LDA, leading to classification into two groups: those who recommend LDA and those who do not. Nurses reinforce provider counseling, follow up with patients, and may fill informational gaps, especially if trained in LDA. Community clinics, which primarily offer preventive care, serve fewer pregnant patients. As a result, even trained providers may lack regular opportunities to counsel on PE and LDA. Therefore, the effectiveness of LDA counseling in these settings is limited by provider capacity and experience. Collectively, the capacities of these five provider types and the influence of resident recommendations affect the likelihood of LDA being recommended (Figure 1).
Information Availability Module
Information availability has a positive influence on women's knowledge (Figure 1). This module replaces the Availability of Information about Preeclampsia to Pregnant Women stock in Model v1 (Appendix 3a) to reflect differing perceptions of information availability across settings. Hospital-based participants reported adequate promotional materials, such as posters, while the community clinic provider noted a lack of informational resources to share with at-risk patients.
Community Providers Home Visiting Program and Doulas Module
Participants noted that some Home Visiting Programs (HVPs) are integrated within hospital systems, allowing referrals from patient advisors or physicians. HVPs aim to promote maternal and child health, strengthen families, and build community well-being [42]. Services are typically delivered in the home, where home visitors provide education and support. However, the landscape in California is complex, with funding from multiple sources: California Department of Public Health (CDPH), California Department of Social Services (CDSS), U.S. Department of Health and Human Services (DHHS), and First 5 Association of California. Home visitors often manage a wide range of issues, including child maltreatment, domestic violence, substance use disorder, and mental health-related challenges. A key limitation identified by a participant was the lack of home visitors trained in LDA treatment, hindering information sharing on PE and LDA. Many women were unaware of HVP availability or their eligibility during early pregnancy, often enrolling too late for effective and timely PE and LDA counseling. Similarly, doulas provide in-home support throughout pregnancy and up to one year postpartum, including emotional, physical, and informational care. While doulas often receive LDA training, they operate independently and their practices often do not have a referral system connected to a hospital, limiting referral pathways. Participants also highlighted challenges related to delayed reimbursements, sometimes up to six months, which had contributed to trained doulas leaving the profession (Figure 1).
Pharmacist Training Module
This module illustrates the change of pharmacists’ status from untrained to trained in LDA treatment. A participant alluded that conflicting advice from providers and pharmacists eroded patients' trust in providers’ recommendations. Pharmacists are trained to advise customers against the intake of aspirin during pregnancy. More trained pharmacists may potentially reduce the knowledge gap between pharmacists and providers and increase adherence to ACOG guidelines on LDA recommendation and prescription (Figure 1).
Recommendations and Referral Process Module
This module outlines the referral and recommendation pathways from family medicine physicians to HVPs and doula services. Referrals can only occur if physicians are aware of these resources. Increased provider awareness is positively associated with earlier referrals and recommendations—ideally prior to PE screening (Figure 1).
Unified Messaging Module
This module monitors the degree of unified messaging, influenced by providers’ adherence to guidelines, the proportion of pharmacists trained in LDA treatment, and the prevalence of correct information circulating within the community. These factors positively contribute to unified messaging, which in turn enhances the knowledge of at-risk pregnant women (Figure 1).
Dynamic Hypothesis
A dynamic hypothesis provides an endogenous explanation of a system’s internal feedback structures that are believed to generate the problem of interest [43]. After building and testing the refined model, we identified key feedback loops influencing LDA initiation and adherence to unveil the system actors with potential influence on LDA uptake (Figure 4). These feedback loops clarify the causal mechanisms and guide scenario testing in the following section. Each loop comprises variables, connecting arrows, polarities, and labels. A positive polarity indicates that an increase in one variable leads to a corresponding increase in the connected variable. In contrast, a negative polarity signifies that an increase in one variable results in a decrease in the connected variable. Self-reinforcing feedback loops, labeled with “R” plus a number, drive exponential growth or decline, as changes in one variable amplify through the system until constrained by a balancing loop or system limits [44]. Conversely, self-correcting balancing loops, labeled with “B” plus a number, guide the system toward a defined or implicit goal.
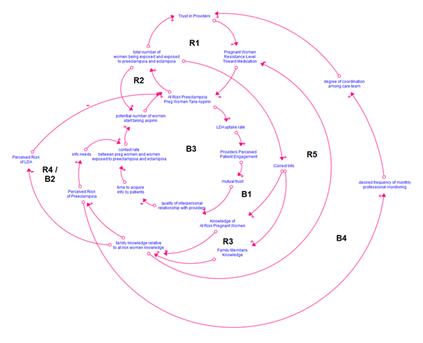
Figure 4: Dynamic Hypothesis of the Low-dose Aspirin Uptake among Women At-risk for Preeclampsia
Starting from the dominant reinforcing R1 loop, Trust in Providers influences women’s resistance toward medication negatively. Lower resistance leads to a higher number of women taking LDA, which in turn sustains or enhances trust in providers. Conversely, increased resistance reduces LDA uptake, decreasing the number of women sharing their experiences within the community, while the contact rate remains constant. This reduction diminishes the motivation of other women to initiate or adhere to LDA treatment (R2). When fewer women disseminate correct information in the community, the knowledge accumulation of women (B1) and their family members (R3) is limited. Because family members heavily influence women’s medication decisions, when their knowledge increases relative to the women’s, women’s risk perception of PE rises, prompting greater information seeking in the community (R3). Conversely, if women’s knowledge outpaces their family’s knowledge, the women’s risk perception will be lower than it would otherwise be, slowing community information seeking (B1), making B1 a balancing constraint. Given the inverse relationships between knowledge and risk perception of LDA, increased family knowledge relative to women’s knowledge reduces risk perception of LDA and non-adherence, forming a positive feedback loop (R4). If women’s knowledge grows faster than their family’s knowledge, risk perception remains stable, and non-adherence persists, resulting in a balancing loop with LDA adherence (B2). Additionally, well-informed family members tend to support medication decisions, lowering women’s resistance and increasing LDA acceptance (R5).
The negative loop B3 is a limiting factor that characterizes the providers’ perception of patient engagement, its influence on the mutual trust between providers and patients, and its impact on the contact rate of women with other women in the community. Greater adherence to LDA fosters stronger mutual trust, enhancing patient-provider relationships and enabling women to seek reliable information directly from providers rather than the community. Strengthening B3 can suppress the reinforcing loops R3 through R5 and the balancing loop B2. It is crucial to allocate resources to promote the growth of R3-R5, B2, and B3 proportionately. Finally, increased risk perception of PE raises demand for more frequent monthly monitoring, fostering closer provider collaboration and further enhancing trust in the provider (B4). Growth in B4 may amplify B3, reinforcing positive patient-provider dynamics. In the next section, we demonstrate the results and analysis of testing various scenarios to increase the stock of women taking LDA.
Scenario Testing and Analyses
Out of the first 20 scenarios with single variable changes we tested (Table 1), scenario 19 showed a significant increase in women taking LDA (Figure 8). The detailed results are presented in Appendix 8.
Table 1: Scenario Testing List
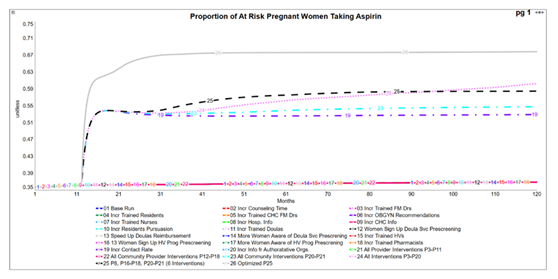
Figure 5: Number of At-risk Women Taking LDA Under Various Scenarios Tested
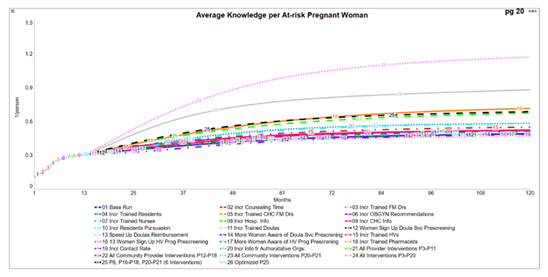
Figure 6: Average Knowledge per At-risk Pregnant Woman Under Various Scenarios Tested
Under the business-as-usual scenario (Scenario 1), the LDA uptake rate and women’s knowledge increased modestly from 35.7% to 36.9% and 1% to 49% over 120 months (Figures 5 and 6). Among all single-variable interventions, Scenario 19 demonstrated the greatest potential impact, increasing the uptake rate to 52.7% at month 120. However, this scenario had little impact on women’s knowledge. Increasing the proportion of pharmacists trained in LDA treatment (P18) was shown to be the most effective intervention in improving women’s knowledge. More substantial increases were observed in multi-variable interventions, particularly Scenarios 23, 24, and 25. The cumulative number of women taking LDA reached 68,500 in Scenario 19, and 69,700, 72,200, and 72,600 in Scenarios 23, 24, and 25, respectively (Figure 7).
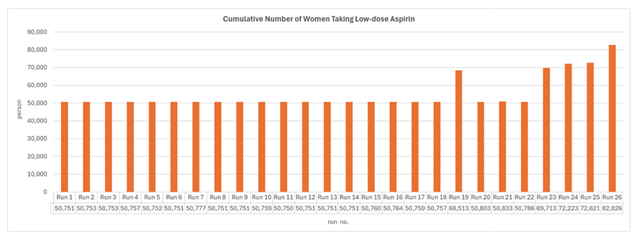
Figure 7: Comparison of the Cumulative Number of Women Taking Low-dose Aspirin under All Runs
Scenario testing indicated that changes in six variables significantly increased the number of women taking LDA: (1) women’s contact rate, (2) information shared by authoritative organizations online, (3) time required for nurses to complete LDA treatment training, (4) timing of pregnant women’s enrollment in the home visiting program, (5) number of home visitors trained in LDA treatment, and (6) awareness of the home visiting program among pregnant women. We optimized these variables to maximize uptake, with upper and lower bounds defined in Appendix 9. The optimization yielded the highest uptake—82,826 women taking LDA. For variables (3) to (5), the optimal values reduced training time for nurses from 36 to 12 months, enrollment time from 4 to 1.5 months into pregnancy, and home visitor training time from 48 to 24 months.
Discussion
Medication decision-making during pregnancy is complex, often influenced by a range of individual, social, and systemic factors. Many public health interventions have struggled to account for this multilevel context, making it difficult to understand the reasons behind their success or failure. The existing literature identifies three primary modalities of LDA interventions: single, multi-modal, and systemic. Single-modal interventions typically involve individual strategies, such as disseminating guidelines, implementing screening protocols, and providing information. Typically, a multimodal intervention consists of multiple elements implemented in an integrated way within an organization, sector, or level (e.g., individual, interpersonal, organizational, community, or societal), and this approach appeared to show better outcomes compared to a single-modal intervention [45, 46]. A systemic intervention is grounded in the principles of expanding the scope of the problem and employing multiple synergistic methodologies to design effective solutions for complex social issues [19]. In this study, we present a novel, systematic inquiry process for developing a simulation model to explore the causal mechanisms influencing the uptake of LDA among pregnant women at risk for PE. Our approach integrates evidence from a literature review, a focus group study with women who have experienced pregnancy complications, and group model building workshops with healthcare providers. The insights gathered through this participatory process were synthesized into a SD simulation model—a method well-suited to managing complexity and demonstrating causality, capturing feedback loops, time delays, and nonlinear relationships. Using the model, we developed a dynamic hypothesis to explain LDA decision-making behavior and tested 20 intervention scenarios. Of these, six showed potential for increasing LDA uptake. We then used the model to optimize the values of these six interventions. Scenarios 2–20 (Figures 5 and 6) represent single-model interventions. Scenarios 21–23 are multimodal interventions, each targeting a single level: providers, patients, or the community. Scenario 24 is a systemic, multimodal intervention that addresses multiple levels and sectors simultaneously, including providers, patients, and the community. Our scenario testing not only projected the impacts of single, multimodal, and systemic interventions, but also identified specific interventions that may outperform the comprehensive Scenario 24. These finding highlights opportunities to prioritize and allocate resources more efficiently to maximize LDA uptake. Overall, our systemic intervention design approach contributed to LDA intervention planning in three main ways: (1) enabling long-term projection of intervention impacts, (2) providing causal tracing capabilities to evaluate and refine intervention strategies, and (3) facilitating scenario testing to identify and prioritize the most resource-effective interventions. Our iterative process—from inquiry to model development, validation, scenario testing, and optimization—enabled us to gain a deep understanding of the system, engage with key stakeholders, and design a systemic intervention with the potential to substantially enhance LDA uptake rates.
Several other studies in the literature have reported on interventions to promote LDA uptake among women at risk of PE. For example, in 2021, the United States Preventive Services Task Force updated its recommendations to include routine blood pressure monitoring throughout pregnancy for women at risk of PE [47] and advised a daily intake of 81 mg of LDA after 12 weeks of gestation for those at high risk [7]. Zhou et al. introduced routine screening prior to the first ultrasound at their California-based facility [14]. Among women identified as high-risk or with two or more moderate-risk factors, LDA self-reported usage was 78% and 68%, respectively, compared to 52% and 22% in unscreened populations. Similarly, Gross et al. implemented nurse-led screening at the first prenatal visit in Wisconsin (n=201) [48]. This approach achieved a 99% screening rate and a 50% increase in LDA recommendation rates within three months. However, the percentage of patients meeting the criteria for LDA use increased by only 1%, suggesting that while provider behavior improved, the eligible patient population remained largely unchanged. Persad et al. developed a provider-focused toolkit aimed at improving LDA recommendations for 94 at-risk women at a New York healthcare facility between 2017 and 2018, resulting in a 54% reduction in the incidence of hypertensive disorders during pregnancy [8]. In Indonesia, Karunia et al. implemented a patient education intervention by distributing informational booklets to 12 high-risk women, leading to a 12% increase in knowledge scores over two months and an improvement in LDA adherence from 89.8% to 95.8% by day 56 of the intervention [9]. Some researchers have proposed a universal LDA implementation as a strategy to circumvent challenges related to screening, prescribing, patient acceptance, and adherence, arguing that resources may be more effectively allocated to patient education. Collectively, these efforts represent single-modal interventions focused on specific aspects such as provider behavior, patient education, or regulatory guidance.
Multi-modal interventions generally targeted provider training. Abbott et al. disseminated educational materials across Boston Medical Center and its affiliated community health centers [49]. This resulted in an 83% and 140% increase in LDA prescriptions among high- and moderate-risk patients, respectively, in 2017 and 2018. Ekawati et al. implemented a comprehensive hypertensive disorder management pathway in Indonesia, involving 16 general practitioners, 24 midwives, and 10 nurses from three primary care clinics. Participants received 20 hours of training, screening checklists, and reminder tools [50]. After one month, 25% of pregnant women (n=114) had been screened; of those, 25% (n=35) were identified as high or moderate risk, and 69% (n=24) of them received an LDA prescription.
Systemic interventions, such as the framework proposed by Tsigas and Magee [51], aim to address PE prevention through broader strategies. These include enhancing patient and provider education, accelerating knowledge dissemination, replicating successful interventions, reshaping public perception of PE, influencing health policy, and fostering collaboration across public and private sectors. However, this systemic approach remains conceptual, lacking specific, measurable outcomes, and mechanisms for evaluating causal relationships. Previous single-modal interventions have typically been limited by small sample sizes, short implementation periods, and a reliance on self-reported outcomes. Multimodal interventions have often focused primarily on provider-centered strategies, potentially overlooking the variability in provider behavior and the complexities of patient decision-making. While systemic approaches offer a more comprehensive framework, many remain at the conceptual stage and require further development into actionable and evaluable plans. Across all these modalities, a common limitation has been the inability to effectively trace and monitor the impact of implemented interventions over time. Our systemic intervention design approach addresses these limitations by expanding the understanding of complex health challenges through the integration of multiple perspectives and active community engagement. This approach supports the development of robust, actionable strategies by leveraging simulation modeling to test, design, optimize, trace, and monitor interventions, enabling continuous learning and adaptation throughout the implementation process.
This study has limitations. Access to patient-level data on LDA use is restricted by stringent IRB protocols, limiting our ability to validate findings. Additionally, the five GMB workshops conducted were insufficient to capture detailed operational dynamics at RUHS. As a result, while we identified key areas for intervention, our analysis does not provide a fully developed implementation strategy; however, it lays a foundation for implementation research to explore and improve upon the impact of the approaches prioritized through this research.
Conclusion
Systemic barriers hinder optimal LDA uptake among women at risk for PE. Our iterative process—from inquiry to model development, validation, scenario testing, and optimization—enabled us to understand the system deeply, engage with key stakeholders, and design a systemic intervention with the potential to enhance LDA uptake rates. By combining local insights with simulation modeling, we identified multi-level interventions that, if implemented, could significantly improve LDA uptake and improve maternal and neonatal outcomes. Participatory SD offers a robust framework for designing context-specific health interventions.
Future directions
Next steps include identifying data requirements for the model and gaining ethical approval to access data. We will then conduct expert interviews at RUHS to enhance our understanding of its operational and organizational dynamics, which will inform model refinement. These efforts will support the development of a comprehensive intervention and implementation strategy tailored to RUHS and its patient population. We expect to learn from refining the strategy during the implementation of the intervention at RUHS and plan to apply this knowledge to design a statewide scale-up in the future.
Acknowledgement
We are deeply grateful to all participants of the focus group study and the group model building (GMB) workshops for their invaluable contributions to this research. We extend our sincere gratitude to our donors, March of Dimes (grant no. 22-FY-169-126) and Christopher Hess Research Fund, for supporting our research. Finally, we thank Mr. Neel Kumar, a first-year student at Occidental College in California, for his technical assistance and diligent notetaking during the virtual GMB workshops.
Ethical Consideration
This research was approved by Stanford University’s Institutional Review Board at Stanford University under protocol number 66458.
Declaration of Competing Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
CRediT Authorship Contribution Statement
Yin Jien Lee: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Data curation, Writing-Original draft preparation, Visualization, Project administration.
Leslie Kowaleswki: Conceptualization, Writing – Review and Editing, Project administration, Funding acquisition. Jeff Gould: Conceptualization, Writing – Review and Editing.
Lindsay du Plessis: Investigation, Writing – Review and Editing.
Bryan Oshiro: Investigation, Writing – Review and Editing.
Melody Moua: Investigation, Writing – Review and Editing.
David K. Stevenson: Writing – Review and Editing, Funding acquisition.
Gary L. Darmstadt: Conceptualization, Formal analysis, Writing – Review and Editing, Supervision.
Data Availability
Appendices are available at https://purl.stanford.edu/ct254xz3088. Complete model documentation can be accessed through https://purl.stanford.edu/hy647zs4234.
References
- C. V. Ananth, K. M. Keyes, and R. J. Wapner. "Pre-eclampsia Rates in the United States, 1980-2010: Age-period-cohort Analysis," (in eng), BMJ 347 (2013): f6564.
- "Pregnancy Mortality Surveillance System." Centers for Disease Control and Prevention (2022).
- K. S. Joseph et al. "Maternal Mortality in the United States: Recent Trends, Current Status, and Future Considerations," Obstetrics & Gynecology 137 (2021): 763-771.
- State of California-Open Data. Hospital Inpatient - Diagnosis, Procedure, and External Cause Codes.
- CODP. Statewide Live Birth Profiles.
- J. Duffy et al. "A Core Outcome Set for Pre-eclampsia Research: An International Consensus Development Study," BJOG: An International Journal of Obstetrics & Gynaecology 127 (2020): 1516-1526.
- "Aspirin Use to Prevent Preeclampsia and Related Morbidity and Mortality: US Preventive Services Task Force Recommendation Statement," JAMA 326 (2021): 1186-1191.
- "ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia," Obstetrics & Gynecology 133 (2019): 1.
- N. W. Ragunanthan, J. Lamb, A. Hauspurg, et al. "Assessment of Racial Disparities in Aspirin Prophylaxis for Preeclampsia Prevention," (in eng), Am J Perinatol (2022).
- D. N. Olson, T. Russell, and A. C. Ranzini. "Assessment of Adherence to Aspirin for Preeclampsia Prophylaxis and Reasons for Nonadherence," (in eng), Am J Obstet Gynecol MFM 4 (2022): 100663.
- P. van Montfort et al. "Low-dose-aspirin Usage among Women with an Increased Preeclampsia Risk: A Prospective Cohort Study," (in eng), Acta Obstet Gynecol Scand 99 (2020): 875-883.
- A. D. A. Lorreia, S. Renaud, and V. M. Pimentel. "Aspirin Acceptance Rate and Perceived Preeclampsia Risk after the Implementation of Universal Screening for Preeclampsia," American Journal of Obstetrics and Gynecology 224 (2021): S184-S184.
- C. N. H. Abheiden, A. V. R. van Reuler, W. W. Fuijkschot, et al. "Aspirin Adherence During High-risk Pregnancies: A Questionnaire Study," Pregnancy Hypertension-an International Journal of Womens Cardiovascular Health 6 (2016): 350-355.
- M. K. Zhou, C. A. Combs, S. Pandipati, et al. "Association of Checklist Usage with Adherence to Recommended Prophylactic Low-dose Aspirin for Prevention of Preeclampsia," (in eng), Am J Obstet Gynecol 228 (2023): 349-351.
- B. Mulder et al. "Risks Versus Benefits of Medication Use during Pregnancy: What do Women Perceive?," Patient Preference and Adherence 12 (2018): 1-8.
- P. Slovic. "Perception of risk," (in eng), Science 236 (1987): 280-285.
- K. L. Wisner et al. "Risk-benefit Decision Making for Treatment of Depression during Pregnancy," (in eng), Am J Psychiatry 157 (2000): 1933-1940.
- H. Nordeng, E. Ystrøm, and A. Einarson. "Perception of Risk Regarding the Use of Medications and Other Exposures during Pregnancy," European Journal of Clinical Pharmacology 66 (2010): 207-214.
- G. Midgley. The Systemic Intervention Approach (2021).
- J. Sterman. Business Dynamics: Systems Thinking and Modeling for a Complex World. McGraw Hill, 2000.
- J. Randers. "Guidelines for Model Conceptualization," in Elements of the System Dynamics Method, J. Randers Ed. Cambridge, Massachusettes, United States: MIT Press 6 (1980): 117-139.
- Y. J. Lee, A. Taft, M. Moua, D. K. Stevenson, and G. L. Darmstadt. "Integrating Evidence and Causal Mapping of Factors Which Influence Medication-Taking Behavior of Pregnant Women at Risk of Hypertensive Disorder: A Scoping Review," Systems 13 (2025): 86.
- J. Kitzinger. "Qualitative Research: Introducing Focus Groups," BMJ 311 (1995): 299-302.
- G. Guest, E. Namey, and K. McKenna. "How Many Focus Groups Are Enough? Building an Evidence Base for Nonprobability Sample Sizes," Field Methods 29 (2017): 3-22.
- M. M. Hennink, B. N. Kaiser, and M. B. Weber. "What Influences Saturation? Estimating Sample Sizes in Focus Group Research," Qualitative Health Research 29 (2019): 1483-1496.
- M. Williams and T. Moser. "The Art of Coding and Thematic Exploration in Qualitative Research" (2019).
- Y. Chun Tie, M. Birks, and K. Francis. "Grounded Theory Research: A Design Framework for Novice Researchers," (in eng), SAGE Open Med 7 (2019): 2050312118822927.
- J. A. M. Vennix. Group Model Building: Facilitating Team Learning Using System Dynamics. Chichester, UK: John Wiley & Sons (1996): 298.
- P. S. Hovmand. Community Based System Dynamics. London: Springer (2014): 104.
- G. Cruden et al. "Leveraging Group Model Building to Operationalize Implementation Strategies Across Implementation Phases: An Exemplar Related to Child Maltreatment Intervention Selection," Implementation Science Communications 5 (2024): 134.
- US Census of Bureau. "Profile - Riverside County, California."
- CDPH. Maternal Health Conditions at Delivery.
- "Health Matters Brief - Maternal Health in Riverside County, California," Riverside University Health System (RUHS) October (2024).
- G. A. Ozin. "Importance and Application of Equilibrium," Journal of Thermodynamics & Catalysis 14 (2023).
- Y. Barlas. "Formal aspects of model validity and validation in system dynamics," System Dynamics Review 12 (1996): 183-210.
- B. Dangerfield. "Optimization of System Dynamics Models," (2009): 9034-9043.
- K. V. Price, R. M. Storn, and J. A. Lampinen. Differential Evolution - A Practical Approach to Global Optimization. Springer (2005).
- P. Schoemaker. "Scenario Planning: A Tool for Strategic Thinking," Sloan Management Review 36 (1995): 25-40.
- S. M. B. Gerdes et al. "Motivation Towards First Trimester Screening for Preeclampsia among Pregnant Women in Denmark: A Cross-sectional Questionnaire Study," Acta Obstetricia et Gynecologica Scandinavica 102 (2023): 1531-1540.
- S. Heimberger et al. "Women’s Perspectives and Attitudes towards the Utility of Angiogenic Biomarkers in Preeclampsia," Pregnancy Hypertension 28 (2022): 109-113.
- L. L. Berry, T. S. Danaher, D. Beckham, R. L. A. Awdish, et al. "When Patients and Their Families Feel Like Hostages to Health Care," Mayo Clinic Proceedings 92 (2017): 1373-1381.
- "California Home Visiting Program (CHVP)." California Home Visiting Program (2025).
- I. Martinez-Moyano. "System Dynamics in Action," Journal of Systems Thinking (2023): 1-16.
- D. H. Meadows. "Leverage Points: Places to Intervene in a System," The Sustainability Institute, 1999.
- R. C.-F. Chan et al. "Nonpharmacological Multimodal Interventions for Cognitive Functions in Older Adults with Mild Cognitive Impairment: Scoping Review," (in eng), JMIR Aging 8 (2025): e70291.
- J. K. Levy et al. "Characteristics of Successful Programmes Targeting Gender Inequality and Restrictive Gender Norms for the Health and Wellbeing of Children, Adolescents, and Young Adults: A Systematic Review," The Lancet Global Health 8 (2020): e225-e236.
- "Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement," JAMA 317 (2017): 1661-1667.
- M. Gross, A. E. Hughes, and K. Sampene. "Operationalizing Aspirin to Reduce Preeclampsia Risk and Related Morbidity and Mortality," Obstetrics and Gynecology 139 (2022): 87S-87S.
- J. Abbott et al. "Provision of Prenatal Aspirin in an Urban Safety-net Population Improves Equity in Perinatal Hypertensive Outcomes," American Journal of Obstetrics & Gynecology 222 (2020): S465.
- F. M. Ekawati, O. Emilia, J. Gunn, et al. "Challenging the Status Quo: Results of An Acceptability and Feasibility Study of Hypertensive Disorders of Pregnancy HDP Management Pathways in Indonesian Primary Care," BMC Pregnancy and Childbirth 21 (2021).
- E. Tsigas and L. A. Magee. "Advocacy Organisations as Partners in Pre-eclampsia Progress: Patient Involvement Improves Outcomes," Best Practice & Research Clinical Obstetrics & Gynaecology 25 (2011): 523-536.
Related PubMed Articles
- Coproducing a health advocate intervention for pediatric liver transplant recipients using a human-centered design.
- Addressing Tobacco-Related Disparities Among Youth Experiencing Homelessness by Engaging Youth Collaborators in Intervention Research: Protocol for a Multimethod, Community-Based Participatory Research Study.
- Integrative review of artificial intelligence applications in nursing: education, clinical practice, workload management, and professional perceptions.
- Co-developing an intervention to facilitate safe and early transition to neonatal home care for very preterm infants: a mixed-method study evaluating the impact of patient and public involvement.
- Digital Informed Consent/Assent in Clinical Trials Among Pregnant Women, Minors, and Adults: Multicountry Cross-Sectional Evaluation of Comprehension and Satisfaction.
- The transformative power of a change laboratory: Experiences from an assessment re-design project in Oman.
- Optimizing mobile app design for older adults: systematic review of age-friendly design.
- Exploring co-design: a systematic review of concepts, processes, models, and frameworks used in public health research.
- Participatory Design for AI-Embedded Artifacts: The Case of ECEB App Design to Fostering Ownership.
