The Athlete's Paradox: Unraveling Coronary Artery Calcification and Cardiovascular Risk
Ali Dakik1, Moied Al Sakan2, Rawad Lakkis1, Hadi Itani3, Abdallah Rebeiz2
1Faculty of Medicine, American University of Beirut, Beirut, Lebanon
2Department of Internal Medicine, Division of Cardiology, American University of Beirut Medical Center, Beirut, Lebanon
3Department of Internal Medicine, Northwell Health, Staten Island, New York, USA
*Corresponding Author: Dr. Moied Al Sakan, Department of Internal Medicine, Division of Cardiology, American University of Beirut Medical Center, Beirut, Lebanon
Received: 22 March 2025; Accepted: 13 April 2025; Published: 15 July 2025
Article Information
Citation: Ali Dakik, Moied Al Sakan, Rawad Lakkis, Hadi Itani, Abdallah Rebeiz. The Athlete's Paradox: Unraveling Coronary Artery Calcification and Cardiovascular Risk. Archives of Clinical and Medical Case Reports 9 (2025): 140-151.
Share at FacebookAbstract
Coronary artery calcifications (CAC) are well-known markers of asymptomatic atherosclerosis and reflect an increased cardiovascular event risk. Large registries and observational studies have demonstrated that endurance athletes carry higher CAC scores than their sedentary and inactive counterparts, raising important questions about the underlying mechanisms, clinical significance, and management strategies. Although regular physical activity is linked to improved cardiovascular health, the presence of high CAC among athletes of high-intensity physical exercise led to further questions regarding this paradoxical phenomenon and its associated implications. This article provides a review of the available evidence and literature of CAC in endurance athletes and its underlying mechanisms. We also provide insights into the types of plaques associated with high-intensity exercise and stratify their risks with cardiovascular disease. Lastly, we determine gaps in the available evidence and present future prospects to determine the long-term cardiovascular implications and assist with management of this subset of population.
Keywords
Cardiovascular disease, Coronary artery calcifications, High-intensity exercise, Athletes, Vigorous exercise.
Article Details
Highlights
- • Coronary artery calcifications increased the risk of developing cardiovascular events.
- • High-intensity exercise athletes tend to have higher rates of coronary artery calcifications compared to sedentary control.
- • Management of athletes with elevated coronary artery calcium score on imaging is similar to those with a sedentary lifestyle.
1. Introduction
Worldwide, cardiovascular diseases (CVDs) continue to be the primary cause of death and morbidity, presenting a serious public health issue. Among the many diagnostic indicators, coronary artery calcification (CAC) has become a key indicator of cardiovascular events, providing insight into subclinical atherosclerosis and general cardiovascular risk [1]. With the use of complex and sophisticated imaging methods, CAC scoring has emerged as a pivotal tool for clinicians to evaluate the severity of atherosclerosis and categorize patients into several risk groups [1]. It is well known that exercising in all its forms (i.e., resistance, aerobic, running) offers substantial health advantages, most notably bettering lipid profiles, decreasing inflammation, improving endothelial function, and overall reducing mortality in those who practice it [2]. However, traditional understandings of CAC as an unmistakable indicator for vascular health have been heavily questioned. Several emerging studies have proved higher CAC incidence, especially in endurance sports athletes, than in those who don't exercise [2]. This stark contradiction between cardiovascular health, exercise, and arterial calcification calls for further investigation, which we attempted to shed light upon. This review highlights the current state of CAC research in the literature, the tools used to measure it, and the apparent paradox between coronary calcification and exercise. We also dwelled on the dual role of CAC in assessing cardiovascular risk in athletes and offer insight to better clinically advise sport regimens in those aiming to mitigate health adversities.
2. Assessment Modalities of Coronary Artery Calcification (CAC)
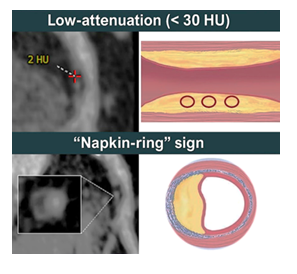
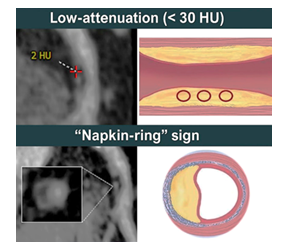
Imaging modalities are integral to evaluating coronary atherosclerosis in athletes, offering crucial insights into both calcified and non-calcified plaque burdens. Non-contrast computed tomography (CT) serves as the gold standard for assessing coronary artery calcification (CAC), providing a reliable and widely accepted method for evaluating atherosclerotic plaque burden [3]. CAC scores are robust predictors of cardiovascular events, with elevated scores correlating strongly with increased risks of myocardial infarction and sudden cardiac death. For example, scores above 400 Agatston units indicate a significantly heightened cardiovascular risk, while scores below 10 are associated with a low 10-year event risk [4]. However, CAC scoring is limited in detecting non-calcified plaques, which may dominate in younger or highly active individuals, potentially underestimating the overall atherosclerotic burden [3]. Coronary CT angiography (CCTA) expands the diagnostic scope of non-contrast CT by encompassing all plaque types—calcified, non-calcified, and mixed—and identifying high-risk features such as low-attenuation plaques (unstable plaque type with lipid necrotic core), napkin-ring signs, and positive remodeling, all of which are strongly associated with future cardiovascular events [5]. Although CAC scoring remains cost-effective for large-scale screening, CCTA provides superior diagnostic precision and accuracy by detecting high-risk plaques and quantifying total plaque burden, a critical advantage for younger or athletic populations where non-calcified plaques predominate [6]. Despite its higher cost, higher radiation exposure, and the need for iodinated contrast agents, CCTA offers invaluable insights into plaque composition and stability, particularly in longitudinal studies evaluating therapeutic outcomes [7, 8].
Figure 1: Example of the plaque low-attenuation (<30 HU) and the “Napkin-ring” sign. Reprinted from: Rampidis GP, Kokkinidis DG, Pakos EE, et al. Role of cardiac CT in the diagnostic evaluation and risk stratification of patients with myocardial infarction and non-obstructive coronary arteries (MINOCA): rationale and design of the MINOCA-GR study. BMJ Open. 2022;12(2):e054698. https://doi.org/10.1136/bmjopen-2021-054698
These insights are of particular importance for athletes as CAC scores alone may fail to capture the interplay between exercise, plaque stability, and cardiovascular risk over time. While non-contrast CT and CAC scoring remain essential for initial risk stratification, CCTA complements these methods by providing a deeper understanding of plaque morphology and its clinical implications. Together, these imaging modalities enable a comprehensive and nuanced approach to life-long cardiovascular risk assessment in athletes [7, 8].
3. Different Plaque Phenotypes and Prognosis
Coronary plaque formation and morphology in athletes differ significantly from sedentary individuals, with non-contrast CT studies frequently revealing a higher prevalence of calcified plaque types in athletes [9]. Calcified plaques formed around 80% of the plaques in athletes, while they comprised only around 30% of the plaques in the sedentary controls, who had predominantly mixed plaques [9]. Studies have favored the predominance of calcified plaques in comparison to other types of plaques in attenuating cardiovascular risks traditionally associated with high CAC. This is explained in cohorts in which achieving high exercise capacity (≥8.2 METs) yielded CAC scores that were inversely correlated with cardiovascular events, indicating a protective effect of fitness even in the presence of CAC [10]. Such findings were reinforced in a large observational study of 21,758 men demonstrating that despite a higher prevalence of CAC scores ≥100 Agatston units among highly active individuals in comparison to sedentary, there was no worsening in all-cause or cardiovascular disease (CVD) mortality [11]. This apparent paradox of increased CAC in highly active individuals without corresponding increases in cardiovascular mortality may be explained by differences in plaque composition. In athletes, CAC often represents stable calcified plaques that have a lower propensity for rupture, whereas mixed or non-calcified plaques—more common in sedentary populations—are more prone to rupture and associated with adverse outcomes [10].
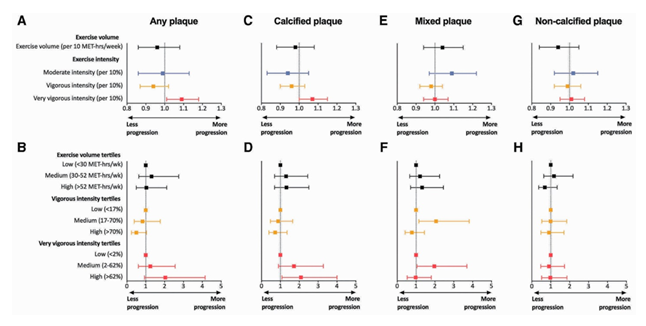
Figure 2: Association Between Different Forms of Plaques and their Progression According to Exercise Volume. Reprinted from: Aengevaeren VL, Mosterd A, Braber TL, et al. Exercise volume versus intensity and the progression of coronary atherosclerosis in middle-aged and older athletes: findings from the MARC-2 study. Circulation. 2023;147(13):993-1003. https://doi.org/10.1161/CIRCULATIONAHA.122.061173.
4. Mechanism of Coronary Calcifications
Several mechanisms have been proposed for the development of coronary artery calcification; the most notable contributors include oxidative stress, systemic inflammation, endothelial dysfunction, and the role of diet and hormones [2, 12].
Oxidative damage and endothelial dysfunction influence CAC progression in athletes. High-intensity exercise induces wall shear stress (WSS), releasing reactive oxygen species (ROS) that bind with nitric oxide (NO) and reduce its bioavailability, impairing proper vascular dilation. Moderate-intensity exercise, on the other hand, limits the concentration of ROS, maintaining adequate non-bonded NO levels that support vascular functioning [12]. The inflammatory response further aggravates vascular damage. Inflammatory markers such as CRP and adhesion molecules like E-selectin and VCAM-1 remain elevated post-exercise and have been linked to worsening endothelial functioning. In certain studies, ultramarathon runners showed significantly elevated inflammatory markers during and after endurance events, corresponding to a higher calcium score than non-athletes [2].
Dietary and hormonal elements also affect CAC score in athletes. Magnesium has an inverse correlation with arterial calcification by behaving as a natural calcium antagonist, maintaining vascular flexibility, and decreasing arterial stiffness. Doses as low as 50 mg/day of magnesium intake are associated with marked reductions in CAC scores and in aortic calcification (p < 0.001) [13]. Hormones, mainly testosterone and dehydroepiandrosterone (DHEA), have shown mixed roles regarding vascular health. Some studies have shown an inverse association between testosterone and CAC, suggesting a protective role in vascular health. Other studies, however, have demonstrated that testosterone therapy may increase non-calcified coronary plaque volume without significantly affecting CAC scores [14]. Catecholamine surges during high-intensity exercise further amplify cardiovascular strain. Levels increase exponentially at higher heart rates, inducing mechanical stress, turbulent blood flow, and prolonged pro-inflammatory changes in monocytes, which promote plaque formation. Excessive parathyroid hormone (PTH) levels have also been implicated in vascular remodeling and calcification. Studies such as the PIVUS and ULSAM cohorts demonstrate strong associations between elevated PTH and increased atherosclerotic burden and nonfatal cardiovascular events [2,15,16].
It is worth mentioning the role of hypertension in exacerbating arterial stiffness and coronary plaques by means of elevating cardiac and inflammatory markers. Exercise-induced hypertension (EIH), defined as a maximal systolic blood pressure of ≥210 mmHg in men or ≥190 mmHg in women during exercise, which is frequently observed in endurance athletes, has been demonstrated in multiple studies to elevate markers such as NT-proBNP, high sensitivity-CRP, and troponin I that reflect sustained myocardial injury. Moreover, long-distance runners with EIH have higher levels of inflammatory markers like endothelin-1 and cTnI, worsening coronary plaques and endothelial cell damage [17-19].
The unique pathophysiological mechanisms mentioned influence coronary plaque phenotypes. Purely calcified plaques, predominant in long-term endurance athletes, are relatively stable and less prone to rupture, illustrating a protective adaptive mechanism in those who exercise. In contrast, non-calcified and mixed plaque types, seen more in non-athletic populations, are associated with higher risks of thrombosis and rupture. While CAC may reduce acute coronary events through plaque stabilization, the overall atherosclerotic risk and chronic inflammatory stimuli necessitate further research to optimize exercise regimens and mitigate cardiovascular burdens [2, 10, 20].
5. Exercise health profiling vs. Non-exercisers
The cardiovascular health profile, along with the coronary calcification status of athletes and sedentary individuals, has been comprehensively studied, showing stark differences between the two in terms of mortality rates, calcification prevalences, and CAC risk assessments. The Copenhagen City Heart Study deduced that jogging 1 to 2.4 hours per week was associated with a 71% reduction in mortality compared to non-joggers [21]. Likewise, a cohort study involving 122,007 patients undergoing exercise treadmill testing showed a strong inverse relationship between cardiorespiratory fitness (CRF) and all-cause mortality, with participants exhibiting extreme CRF levels (≥2 SDs above the mean) having the lowest risk-adjusted mortality rates [22]. Further meta-analyses further back up these findings, indicating that elite athletes encounter significantly fewer cardiovascular disease (CVD) incidents and mortality compared to the general population (standardized mortality ratio: 0.67) [23]. On the other hand, heavy exercise has been linked to higher coronary plaque prevalence compared to those who don't. One study showed that middle-aged runners displayed a 44.3% prevalence of atherosclerosis vs. 22.2% in controls, with runners commonly having more calcified plaque type (72.7%) while most sedentary controls demonstrate mixed-type plaques (61.5%)
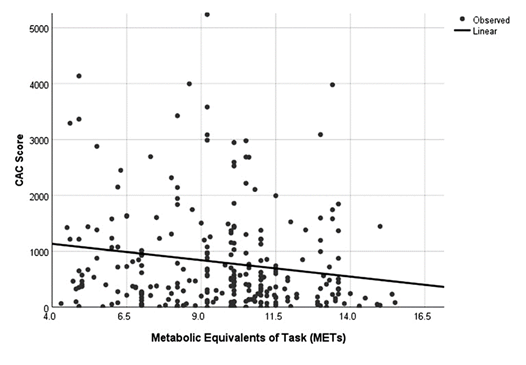
CAC risk is influenced by lifestyle factors. The SCAPIS study concluded that moderate-to-vigorous physical activity (MVPA) decreases CAC risk, while sedentary habits increase its progression. Individuals engaging in MVPA (>2% of daily activity) had a lower CAC risk, in comparison to the sedentary behavior group (>70% of the cumulative daily time), which exhibited higher CAC progression [25]. A study of master's endurance athletes showed that male athletes had a higher prevalence of atherosclerotic plaques (44.3% vs. 22.2%; P = 0.009) and calcified plaques (72.7% vs. 38%) than sedentary controls. Additionally, 11.3% of athletes had CAC scores ≥300 Agatston units compared to 0% of controls, with a longer training history being an independent predictor of CAC ≥70th percentile (OR = 1.08 per training year; 95% CI: 1.01–1.15; P = 0.016) (9). Lastly, in patients with established CAD, higher exercise capacity has been linked to lower CAC scores, with every 1-MET increase in capacity being linked to a 66.2 CAC unit reduction [10]. Participants achieving ≥8.2 METs had substantially fewer cardiovascular events (4.25%) compared to those with lower exercise efficiency (12.9%; P = 0.038). Interestingly, however, both moderate and high-intensity exercise volumes provided similar reductions in CAC, suggesting that CRF, rather than the intensity of the exercise, is the central determinant of cardiovascular well-being [11].
Figure 3: The relationship between CAC score and achieved METs. Reprinted from: Malik A, Zhao Y, Budoff M, et al. Exercise capacity, coronary artery fatty plaque, coronary calcium score, and cardiovascular events in subjects with stable coronary artery disease. J Am Heart Assoc. 2020;9(7):e014919. https://doi.org/10.1161/JAHA.119.014919
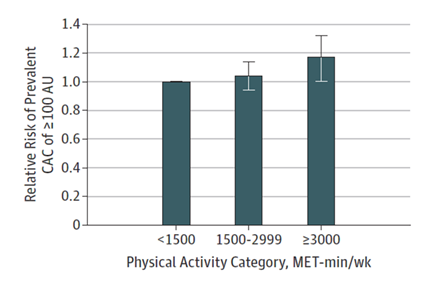
Figure 4: Prevalence of CAC and its relative risk according to stratification of physical activity category. Reprinted from: DeFina LF, Radford NB, Barlow CE, et al. Association of all-cause and cardiovascular mortality with high levels of physical activity and concurrent coronary artery calcification. JAMA Cardiol. 2019;4(2):174-181. https://doi.org/10.1001/jamacardio.2018.4628.
6. Extreme Exercise Profiling vs. Non-Extreme Exercise
Cardiovascular benefits have a curvilinear pattern of association with exercise intensity, with the healthiest outcomes favoring moderate-intensity physical training. A study of 21,266 young participants revealed that Cecreased with exercise volumes of 764 to 1,091 MET-min/week, but higher levels of physical activity did not provide further risk reduction [26]. This trend aligns with findings from the Copenhagen City Heart Study, in which light joggers (HR: 0.22) and moderate joggers (HR: 0.66) exhibited the greatest reductions in mortality, whereas those who jogged strenuously had mortality rates (HR: 1.97) comparable to sedentary individuals [21]. Hence, an overall U-shaped curve exists between exercise dose and mortality, with moderate exertions yielding the most favorable results. Despite the cardiovascular benefits of exercise, extreme endurance exercise (EEE) is linked to greater coronary artery calcification (CAC). In marathon runners, high-EEE participants were nine times more likely to have CAC >0 and 10 times more likely to exceed the 50th percentile for CAC compared to low-EEE runners, with 73.3% and 33% of high-EEE athletes showing CAC >0 and >100, respectively, versus 23.1% and 11.5% in low-EEE athletes [27]. Similarly, in a cohort of 284 athletes, those exceeding 2,000 MET-min/week had significantly higher CAC prevalence (68% vs. 43%) and plaque burden (77% vs. 56%) compared to participants exercising <1,000 MET-min/week [10]. Furthermore, a study conducted by Gerber et al. has demonstrated that the aHR for those with CAC and higher CRF was 4.68, compared to those with no CAC and lower CRF (aHR=2.22) and for CAC and lower CRF (aHR=3.72). As for coronary heart disease (CHD), the HRs were found to be 9.98, 2.28, and 5.52, respectively. For mortality, the first group carried the lowest risk (aHR = 1.15), and the last group carried the highest risk (aHR= 3.14) [28]. Exercise-induced hypertension (EIH) also appears to influence plaque formation in extreme exercisers. Marathon runners with EIH had significantly higher CAC scores (42.6 ± 67.8 vs. 2.8 ± 6.0; P < 0.05) and plaque prevalence, including cases of stenosis (12 vs. 1; P < 0.05), compared to normotensive runners [23].It is important to highlight that even though some studies showed that vigorous-intensity exercise was independently associated with elevated CAC (aOR = 1.47, 95% CI: 1.14–1.91) and plaque presence (aOR = 1.56, 95% CI: 1.17–2.08), the most active group exhibited a favorable plaque phenotype, with a higher proportion of calcified plaques (38% vs. 16%; aOR = 3.57, 95% CI: 1.28–9.97) and fewer mixed plaques (48% vs. 69%; aOR = 0.35, 95% CI: 0.15–0.85), suggesting greater plaque stability and reduced rupture risk despite increased CAC prevalence [10]. Notably, there exist differences even between the most “elite” exercise practitioners and the high performers, with elite athletes having cardiorespiratory fitness (CRF) levels that confer considerable survival advantages, especially in older cohorts [22]. Among older adults (≥70 years), elite athletes exhibited a 29% reduction in all-cause mortality compared to high performers (adjusted HR = 0.71, 95% CI: 0.52–0.98; P = 0.04), while no statistical difference was found in the younger population between both samples. Similarly, hypertensive elite athletes showed a 30% lower mortality risk compared to their high-performing counterparts (adjusted HR = 0.70, 95% CI: 0.50–0.99; P = 0.05). These findings underscore the long-term benefits of sustained fitness in mitigating age- and hypertension-related cardiovascular risks [22].
7. Intensity of Exercise vs. Volume of Exercise’s Effect on CAC Levels
Exercise intensity influences coronary artery calcification (CAC) more significantly and consistently than volume. A Korean cohort study of 25,485 adults revealed that higher-intensity physical activity was linked to greater CAC progression, with the "health-enhancing" group (≥3000 MET-min/week) exhibiting significantly higher 5-year CAC progression compared to less active individuals [29].
The MARC-2 study, which followed 289 middle-aged men over 6.3 years, demonstrated that exercise volume was not significantly associated with CAC progression. Instead, vigorous-intensity activity (6–9 MET-hours/week) was linked to a smaller increase in CAC (β = −0.05 per 10% increase, P = 0.02), while very vigorous-intensity exercise (≥9 MET-hours/week) was associated with greater CAC progression (β = 0.05 per 10% increase, P = 0.01) (30). Extreme intensity activity, however, following the results previously mentioned in this review, increased the odds of both calcified plaque (adjusted odds ratio [aOR] = 1.07, 95% CI: 1.00–1.15) and overall plaque progression (aOR = 1.09, 95% CI: 1.01–1.18), respectively [30].
Similar findings were concluded in the Cooper Clinic Longitudinal Study, involving 8,771 participants over 7.8 years, which found that physical activity volume did not predict CAC progression to clinically meaningful thresholds (≥100 Agatston units [AU]) [31]. Such data is in accordance with studies on recreational athletes that suggested that exercise volume alone does not consistently predict CAC changes. For example, after 4.1 years of follow-up in subjects with or without CAC progression, there was no significant difference in exercise volume between the two groups. (68 [33–122] vs. 50 [34–82] MET-hours/week; P = 0.16) [32].
Taking into consideration the baseline CAC level in individuals influences calcification progression and mortality greatly. Healthy men with a baseline of CAC between 1-99 AU exhibited reduced calcification development in all physical activity levels compared to participants with CAC levels ≥ 100 AU when subjected to the same exercise regimens (P = 0.04) (67). However, regardless of the volume of training, those with lower CAC levels displayed reduced mortality rates, highlighting the protective effect of exercise despite CAC presence [31].
Important deductions regarding the ideal balance of intensity and volume spent exercising pertaining to coronary calcifications have risen to the surface of recent literature. A study of 25,801 healthy men explored the influence of exercise intensity and duration on CAC. High-intensity physical activity (≥8 METs), when performed not more than 5 hours a week (RR = 0.92, CI: 0.88–0.97, P = 0.003), decreased significantly the risk of elevated CAC (Relative Risk [RR] = 0.93, 95% CI: 0.88–0.98, P = 0.004). However, increased exercise durations (≥5 hours/week) trended toward worsening CAC risk, though not statistically significant (RR = 1.07, CI: 0.98–1.17, P = 0.14) [33].
The highest prevalence of high calcification scores (CAC ≥100 AU) was observed in men engaging in low-intensity physical activity (<8 METs) for prolonged periods (≥5 hours/week), while the lowest prevalence occurred in those performing high-intensity activity (≥3000 MET-min/week) for less than 5 hours/week [33]. Additionally, individuals in the highest physical activity group exhibited better glucose and lipid profiles than those in the lowest group (<1500 MET-min/week), emphasizing the benefits of high-intensity exercise [33].
Thus, one can conclude that exercise volume can be used to gauge CAC prevalence, and relying on intensity is a good measure to understand CAC progression. The findings above highlight the importance of urging clinicians to prioritize intensity-driven exercise regimens for those with elevated CAC for optimal cardiovascular health outcomes.
8. Clinical Relevance of Coronary Atherosclerosis in Athletes
Assessing the clinical risk associated with CAC in athletes:
Is an elevated CAC level truly a marker of elevated cardiovascular risk, or merely a benign finding in this population? Most of the studies chosen to evaluate the relationship between exercise intensity or volume and CAC scores were either prospective cohort studies or cross-sectional reviews. Regardless of the type, most of the studies ended up showing a similar relationship between CAC scores and exercise intensity. This seems to be a U-shaped relationship, meaning that CAC scores tend to decrease with light or moderate exercise and increase as exercise intensity increases further to severely intense exercise [1, 21]. This was seen in a prospective cohort study by Aengevaren et al. that illustrated a U-shaped relationship between CAC and exercise where vigorous was associated with less CAC progression, whereas very vigorous exercise was associated with greater CAC progression [10].
Studies by Mohlenkamp et al. and Merghani on the other hand showed no difference in the prevalence of elevated CAC scores (above 0) in athletes when compared to sedentary counterparts [4, 9]. However, the cross-sectional studies by Aengevaren et al. and DeFina et al. all showed an increase in the prevalence of very elevated CAC scores (over 100) in active athletes when compared to sedentary counterparts [4, 21, 33].
Similarly, in a study by Lavie et al. athletes competing in EEE (extreme endurance exercise) had a higher prevalence of CAC than those who only completed shorter races; they were 9-10 times more likely to have CAC at the 50th percentile or greater and scores greater than 0 compared with the lower distance runners after controlling for the covariates [1].
On average, athletes tend to have normal CAC scores, but it was seen that a moderately or severely elevated CAC score is significantly more prevalent in male athletes compared to their male counterparts, as shown in a study by Masson et al. These differences were limited to male participants and were not seen in females. In a prospective cohort study by Sung et al. where 25 485 participants were followed and analyzed for a period of 5 years, higher physical activity was seen to be associated with higher CAC levels and a faster progression of coronary artery calcification regardless of baseline CAC status [29].
In general, it seems that the association between CAC progression, if found, is to be more strongly influenced by exercise intensity rather than exercise volume as previously mentioned.
This distinction was highlighted in a study by Aengevaeren et al., which demonstrated that exercise volume was not significantly related to the progression of coronary atherosclerosis or coronary calcification. In contrast, higher exercise intensity was associated with accelerated CAC progression [10]. On another hand, a prospective cohort by Kleiven et al. showed no relationship between coronary artery calcification and the amount of exercise per week in endurance athletes and suggests that baseline CAC and other characteristics such as age are better predictors of CAC progression than exercise intensity [32].
Exercise seems to have an effect on not only the CAC score but also atherosclerosis in general. In accordance with what we mentioned in the review, studies showed more diffuse distribution of calcified plaques throughout the coronary tree of athletic males compared to sedentary males and even had a higher prevalence of luminal stenosis when compared to their counterparts [17].
On top of that, studies like the one by Aegenevaren et al. demonstrated that the proportion of calcified plaques increases with higher exercise intensity. Among athletes engaging in more than 2000 METs/week of exercise, the prevalence of calcified plaques was approximately 80%, compared to around 60% in those performing less than 1000 METs/week [4].
Although calcified plaques might be cardioprotective because of their stability, these plaques can cause significant luminal stenosis, which can itself lead to further complications such as myocardial fibrosis and nonsustained ventricular tachycardia, as was seen in this study [4, 34]. This suggests that mechanisms different from plaque rupture can explain the cardiovascular mortality of these intense athletes.
In terms of cardiovascular risk, there has been some conflicting evidence among different studies. An observational study by DeFina et al. highlighted the interplay between coronary artery calcium (CAC) levels, physical activity, and mortality risk. Among men with CAC scores below 100 Agatston units (AU), those engaging in high levels of physical activity (≥3000 MET-minutes per week) were about half as likely to die from any cause compared to men with lower activity levels (<1500 MET-minutes per week) [11].
In contrast, in men with CAC scores ≥100 AU, those who maintained high activity levels did not experience a significant increase in all-cause mortality. However, among the least active men, those with CAC scores ≥100 AU had double the cardiovascular mortality risk compared to those with CAC scores <100 AU [11]. These findings suggest that while elevated CAC in sedentary individuals is linked to higher cardiovascular risk, high physical activity levels may mitigate this risk, emphasizing the protective role of exercise even in individuals with subclinical atherosclerosis? [11].
Similar findings were found by Arnson et al. who discovered an inverse relationship between adverse cardiovascular events and the amount or intensity of exercise performed in athletes with a CAC score above 0 and especially in patients with a CAC score over 400, no relationship was depicted between exercise intensity and cardiovascular events in athletes with a CAC score of 0 [20]. This paradox becomes apparent as the aforementioned Copenhagen study’s U-shaped relationship depicted similar mortality rates between sedentary non-joggers and strenuous joggers, while light and moderate joggers were found to have a lower mortality rate which is similar to the relationship found between CAC and exercise intensity discussed above [35]. Therefore, as we can see, it is still uncertain whether coronary artery calcification is cardioprotective or actually a predisposing factor for cardiovascular disease [29].
In summary, studies consistently show a U-shaped relationship between exercise intensity and CAC scores, with moderate exercise associated with lower scores and intense exercise linked to higher progression. Athletes tend to have a higher prevalence of calcified plaques, which are denser and more stable, potentially reducing the risk of rupture compared to mixed plaques seen in sedentary individuals. These findings highlight distinct differences in plaque prevalence and composition between active and sedentary populations.
Table 1: Summary of Key Findings of CAC and its Associated Clinical Risk.
|
Study |
Study Type |
Objective |
Participants Number |
Follow up Period |
Key Findings |
Year |
|
Arnson et al. [20] |
Retrospective cohort |
Assess the correlations among CAC, self-reported exercise, and mortality in asymptomatic patients. |
10,690 |
8.9 +/- 3.5 years |
Exercise may play a protective role among patients with high CAC scores. Reported minimal or no exercise substantially increases the clinical risk. |
2017 |
|
Mohlenkamp et al. [36] |
Prospective cohort |
Previous studies were performed on marathon runners ≥50 years of age who are less likely to have advanced CAD and suffer from ischemic events. |
1,188 |
6 +/- 1 year |
Marathon runners with myocardial fibrosis develop higher troponin values during the race than those without. Increased CAC and myocardial fibrosis lead to higher coronary event rates. All-cause mortality in marathon runners is similar to those with risk factors. |
2014 |
|
LaMonte el at. [37] |
Prospective cohort |
Higher exercise tolerance is associated with a lower incidence of CHD events in asymptomatic individuals with significant subclinical coronary atherosclerosis based on the presence of CAC scores ≥100. |
710 |
3.5 +/- 1.4 years |
Maximal exercise tolerance adds additional prognostic information. An exercise tolerance level of ≥10 METs identifies patients who are at lower risk for developing clinical manifestations of CHD across a range of CAC scores ≥100. |
2006 |
|
Radford et al. [38] |
Retrospective cohort |
Identify the presence of a dose-response relationship between cardiorespiratory fitness and CVD risk across CAC categories in a large, generally healthy population of men. |
8,425 |
8.4 years |
Attenuation of CVD risk at all CAC levels with higher cardiorespiratory fitness. |
2018 |
|
Defina et al. [11] |
Prospective cohort |
Assess the correlation among high levels of physical activity, CAC, and mortality risk. |
21,758 |
16 years |
A high level of physical activity is associated with prevalent CAC but not with increased all-cause or CVD mortality |
2019 |
|
Gerber et al. [28] |
Prospective cohort |
Examining the association between cardiorespiratory fitness or moderate-to-vigorous physical activity and CAC with outcomes and determine CAC incidence. |
3,141 |
13-14 years |
Cardiorespiratory fitness and moderate-to-vigorous physical activity are inversely associated with CAC and they did not decrease the risk of cardiovascular disease. |
2025 |
9. Management of Athletes with Elevated CAC
So what are the recommendations and management strategies in treating athletes with elevated CAC scores? In general, there are not many studies tackling this specific issue, and there seem to be no recommendations specific for athletes with elevated CAC scores.
Based on an article by Lechner et al., recommendations for athletes with elevated CAC are similar to those for the general population, which include, but not limited to, avoiding refined sugars, trans fatty acids, and cigarette smoke [39]. In addition, good, consistent sleep patterns are recommended, as well as lipid-modulating therapy such as statins when indicated [2]. In addition, moderate-level exercise is generally encouraged in patients with all CAC levels unless there is any indication against it. Individuals interested in participating in competitive sports require cardiovascular evaluation by their sports cardiologist regardless of CAC levels [2].
One important factor to take into consideration in athletes is the phenomenon of hypertensive response to exercise, which is defined most commonly as having blood pressure values of 210/105 mmHg for men, 190/105 mmHg for women, and 220/210 mmHg for athletes at peak exercise [18]. It is still uncertain whether it should be treated but has been linked to adverse cardiovascular events in exercising individuals [40]. Data suggests that ARBs or ACE inhibitors could be one of the mainstay treatments for this condition, as elevated angiotensin II was shown to be elevated in individuals with exaggerated blood pressure response to exercise [41]. However, more data and clinical trials are needed to make a conclusion on this matter [40].
In addition, as previously mentioned, the Framingham study depicts an inversely dose-dependent relationship between magnesium intake and coronary artery calcification, whereas increased magnesium intake was correlated with progressively lower CAC scores [13]. This could prompt patients with elevated CAC scores to take magnesium as a treatment, which could lower their CAC levels and, in addition, their cardiovascular risks.
In conclusion, managing elevated CAC scores in athletes follows general population guidelines, including lifestyle changes, moderate exercise, and lipid-lowering therapy when indicated. Unique considerations, such as hypertensive responses to exercise and the potential benefits of magnesium supplementation, highlight the need for further research. Individualized care and sports cardiology evaluations are key to optimizing cardiovascular health in these individuals.
10. Future Directions and Research Gaps
As observed, most of the articles we have taken into account eventually lead to the same conclusion and have similar findings. Most notably, the U-shaped relationship between CAC scores and exercise intensity, as well as the discrepancy in plaque composition between athletes and sedentary people, where athletes tend to have plaques richer in calcium, which are hypothesized to be more stable. Nonetheless, there are still notable limitations regarding research about this topic.
First of all, a lot of the studies seem to shift their focus on male athletes, with female athletes being less studied and represented; one of the studies proved that a relationship between CAC and exercise intensity exists but failed to depict the same regarding women athletes [42]. So, despite having a replicable correlation between coronary artery calcification and exercise intensity, we are still unaware whether the same applies to the female population, and therefore more data is required. In addition, in most studies, many confounders that might affect the findings of these studies were not taken into account. Some of these are, but are not limited to: the use of performance-enhancing drugs, which were proven to be related to the acceleration of atherosclerosis [24], family history, diet, and lifestyle. Another thing to note is that in many of these studies, the frequency and intensity of exercise are self-reported by the studied subjects, which can inaccurately skew the results of these studies.
In addition, many of these studies are cross-sectional, which limits their ability to establish correlative relationships between variables. Furthermore, there is a notable lack of long-term prospective cohort studies on this topic, which could provide insights and uncover outcomes that the authors may not have anticipated. As was established, there are still no specific treatment plans or guidelines regarding managing athletes with coronary artery calcifications [43]. Although many possible mechanisms regarding coronary artery calcification in athletes were hypothesized, the literature still did not establish a clear-cut mechanism regarding this process, which could be essential in putting a treatment protocol to manage this specific population.
In summary, while research points to a U-shaped relationship between CAC scores and exercise intensity, along with more stable calcium-rich plaques in athletes, significant gaps remain. These include limited data on female athletes, overlooked confounders, and a reliance on self-reported exercise data. More robust, long-term studies are needed to better understand this phenomenon and guide effective management.
11. Conclusion / Limitations
In summary, coronary artery calcification (CAC) presents a unique paradox in athletes, particularly those engaged in high-intensity endurance sports. The present review summarizes current evidence about the intriguing dynamics of coronary artery plaques among athletes, offering insights into their composition, prevalence, and potential implications for cardiovascular health. Data from the literature highlights the complexity of atherosclerosis in this unique population and raises pertinent questions regarding the interplay between physical activity, plaque morphology, and cardiovascular risk. To further understand the mechanisms behind the development and progression of CAC, future research should try to involve different populations, including female athletes. To create tailored guidelines for controlling cardiovascular risk in athletes and guarantee that they may continue to reap the benefits of physical activity while reducing potential health concerns, it will be imperative to address these research gaps.
Central illustration:
Key Highlights of The Article
|
Key Concept |
Details |
|
Exercise and CAC Paradox |
Despite cardiovascular benefits, endurance exercise is linked to increased CAC. |
|
Imaging Techniques |
CT and CCTA are essential for assessing coronary atherosclerosis in athletes. |
|
Stable vs. Non-Calcified Plaques |
Athletes have more stable calcified plaques compared to sedentary individuals. |
|
Impact on Mortality |
Increased CAC in athletes does not correlate with higher mortality. |
|
Mechanisms Behind Plaque Stability |
Exercise-induced hypertension, oxidative stress, inflammation, and hormonal factors promote stable plaques over rupture-prone plaques. |
|
Exercise Intensity and Cardiovascular Benefits |
Moderate exercise provides the greatest benefits; extreme endurance exercise increases CAC but favors stable plaque formation. |
|
U-Shaped Relationship |
Increased CAC in athletes does not correlate with higher mortality. |
|
Pathophysiology of CAC |
|
Wall shear stress à release of ROS à binds with NO à impaired vasodilation |
|
Elevated inflammatory markers post-exercise à endothelial dysfunction à vascular damage |
|
Low magnesium àdecreased calcium antagonism àdecreased vascular flexibility à increased arterial stiffness |
|
Catecholamine surge during exercise à mechanical stress à turbulent blood flow à prolonged pro-inflammatory changes à plaque formation |
Evidence Gaps
|
Most studies focus on male athletes making it unclear if the CAC-exercise relationship applies to women. |
|
Factors such as performance-enhancing drugs, diet, lifestyle, and genetics are often not taken into consideration. |
|
The majority of the studies are observational, thus limiting the application to determine a causal association. |
|
Long-term outcomes have not been assessed due to a lack of long-term prospective cohort or interventional studies. |
|
No clear consensus or mechanism exists regarding CAC induced by exercise. |
References
- Lavie CJ, Hecht HF, Wisloff U. Extreme Physical Activity May Increase Coronary Calcification, But Fitness Still Prevails. Mayo Clin Proc Innov Qual Outcomes 3 (2019): 103-135.
- Zambrano A, Tintut Y, Demer LL, et al. Potential mechanisms linking high-volume exercise with coronary artery calcification. Heart 109 (2023): 1139-1145.
- Sun Z, Silberstein J, Vaccarezza M. Cardiovascular Computed Tomography in the Diagnosis of Cardiovascular Disease: Beyond Lumen Assessment. J Cardiovasc Dev Dis 11 (2024).
- Aengevaeren VL, Mosterd A, Sharma S, et al. Exercise and Coronary Atherosclerosis Observations, Explanations, Relevance, and Clinical Management. Circulation 141 (2020): 1338-1350.
- Serruys PW, Hara H, Garg S, et al. Coronary Computed Tomographic Angiography for Complete Assessment of Coronary Artery Disease: JACC State-of-the-Art Review. J Am Coll Cardiol 78 (2021): 713-736.
- Chow ALS, Alhassani SD, Crean AM, Small GR. Coronary ct angiography guided medical therapy in subclinical atherosclerosis. J Clin Med 10 (2021): 1-14.
- Joner M, Koenig W. Risk prediction by non-invasive coronary imaging: We are not there yet! Eur Heart J 39 (2018): 942-944.
- Lakshmanan S, Rezvanizadeh V, Budoff MJ. Comprehensive plaque assessment with serial coronary CT angiography: translation to bedside. Int J Cardiovasc Imaging 36 (2020): 2335-2346.
- Merghani A, Maestrini V, Rosmini S, et al. Prevalence of Subclinical Coronary Artery Disease in Masters Endurance Athletes with a Low Atherosclerotic Risk Profile. Circulation 136 (2017): 126-137.
- Aengevaeren VL, Mosterd A, Braber TL, et al. Relationship between Lifelong Exercise Volume and Coronary Atherosclerosis in Athletes. Circulation 136 (2017): 138-148.
- Defina LF, Radford NB, Barlow CE, et al. Association of All-Cause and Cardiovascular Mortality with High Levels of Physical Activity and Concurrent Coronary Artery Calcification. JAMA Cardiol 4 (2019):174-181.
- Wang YX, Liu H Bin, Li PS, et al. ROS and NO Dynamics in Endothelial Cells Exposed to Exercise-Induced Wall Shear Stress. Cell Mol Bioeng 12 (2019): 107-120.
- Hruby A, O’Donnell CJ, Jacques PF, Meigs JB, Hoffmann U, McKeown NM. Magnesium intake is inversely associated with coronary artery calcification: The framingham heart study. JACC Cardiovasc Imaging 7 (2014): 59-69.
- Budoff MJ, Ellenberg SS, Lewis CE, et al. Testosterone treatment and coronary artery plaque volume in older men with low testosterone. JAMA - J Am Med Assoc 317 (2017): 708-716.
- Hagström E, Michaëlsson K, Melhus H, et al. Plasma-parathyroid hormone is associated with subclinical and clinical atherosclerotic disease in 2 community-based cohorts. Arterioscler Thromb Vasc Biol 34 (2014): 1567-1573.
- Shah AB, Bechis MZ, Brown M, et al. Catecholamine response to exercise in patients with non-obstructive hypertrophic cardiomyopathy. J Physiol 597 (2019): 1337-1346.
- Sung J, Cho SJ, Choe YH, et al. Prevalence of coronary atherosclerosis in asymptomatic middle-age men with high aerobic fitness. Am J Cardiol 109 (2012): 839-843.
- Ghidoni C, Kruzik M, Rossi VA, et al. Definitions for Hypertensive Response to Exercise. Cardiol Rev 32 (2024).
- January CT, Wann LS, Calkins H, et al. AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart R. Circulation 140 (2019): e125-151.
- Arnson Y, Rozanski A, Gransar H, et al. Impact of Exercise on the Relationship Between CAC Scores and All-Cause Mortality. JACC Cardiovasc Imaging 10 (2017): 1461-1468.
- Schnohr P, O’Keefe JH, Marott JL, et al. Dose of jogging and long-term mortality: The Copenhagen City heart study. J Am Coll Cardiol 65 (2015): 411-419.
- Mandsager K, Harb S, Cremer P, et al. Association of Cardiorespiratory Fitness With Long-term Mortality Among Adults Undergoing Exercise Treadmill Testing. JAMA Netw open 1 (2018): e183605.
- Lucia A. Elite athletes live longer than the general population: a meta-analysis. Mayo Clin Proc 89 (2014): 1195-1200.
- Baggish AL, Levine BD. Coronary Artery Calcification Among Endurance Athletes: “Hearts of Stone”. Vol. 136, Circulation. United States; (2017): 149-151.
- Ekblom-Bak E, Börjesson M, Ekblom Ö, et al. Accelerometer derived physical activity and subclinical coronary and carotid atherosclerosis: cross-sectional analyses in 22 703 middle-aged men and women in the SCAPIS study. BMJ Open. Nov;13 (2023): e073380.
- Maessen MFH, Verbeek ALM, Bakker EA, et al. Lifelong Exercise Patterns and Cardiovascular Health. Mayo Clin Proc 91 (2016): 745-754.
- Lin J, DeLuca JR, Lu MT, et al. Extreme Endurance Exercise and Progressive Coronary Artery Disease. J Am Coll Cardiol 70 (2017): 293-295.
- Gerber Y, Gabriel KP, Jacobs DRJ, et al. The relationship of cardiorespiratory fitness, physical activity, and coronary artery calcification to cardiovascular disease events in CARDIA participants. Eur J Prev Cardiol 32 (2025): 52-62.
- Sung KC, Hong YS, Lee JY, et al. Physical activity and the progression of coronary artery calcification. Heart 107 (2021): 1710-1716.
- Aengevaeren VL, Mosterd A, Bakker EA, et al. Exercise Volume Versus Intensity and the Progression of Coronary Atherosclerosis in Middle-Aged and Older Athletes: Findings from the MARC-2 Study. Circulation 147 (2023): 993-1003.
- Shuval K, Leonard D, DeFina LF, et al. Physical Activity and Progression of Coronary Artery Calcification in Men and Women. JAMA Cardiol 9 (2024): 659-666.
- Kleiven Ø, Bjørkavoll-Bergseth MF, Omland T, et al. Endurance exercise training volume is not associated with progression of coronary artery calcification. Scand J Med Sci Sport 30 (2020): 1024-1032.
- Pavlovic A, DeFina LF, Leonard D, et al. Coronary artery calcification and high-volume physical activity: role of lower intensity vs. longer duration of exercise. Eur J Prev Cardiol 31 (2024): 1526-1534.
- Kim YJ, Park KM. Possible Mechanisms for Adverse Cardiac Events Caused by Exercise-Induced Hypertension in Long-Distance Middle-Aged Runners: A Review. J Clin Med 13 (2024).
- Ozemek C, Laddu DR, Lavie CJ, et al. An Update on the Role of Cardiorespiratory Fitness, Structured Exercise and Lifestyle Physical Activity in Preventing Cardiovascular Disease and Health Risk. Prog Cardiovasc Dis 61 (2018): 484-490.
- Möhlenkamp S, Leineweber K, Lehmann N, et al. Coronary atherosclerosis burden, but not transient troponin elevation, predicts long-term outcome in recreational marathon runners. Basic Res Cardiol 109 (2014).
- LaMonte MJ, FitzGerald SJ, Levine BD, et al. Coronary artery calcium, exercise tolerance, and CHD events in asymptomatic men. Atherosclerosis 189 (2006): 157-162.
- Radford NB, DeFina LF, Leonard D, et al. Cardiorespiratory fitness, coronary artery calcium, and cardiovascular disease events in a cohort of generally healthy middle-age men: Results from the cooper center longitudinal study. Circulation 137 (2018): 1888-1895.
- Lechner K, Halle M, Scherr J, et al. Exercise recommendations in athletes with coronary artery calcification. Eur J Prev Cardiol 27 (2020): 882-884.
- Kim D, Ha J-W. Hypertensive response to exercise: mechanisms and clinical implication. Clin Hypertens 22 (2016): 16-19.
- Shim CY, Ha JW, Park S, et al. Exaggerated Blood Pressure Response to Exercise Is Associated With Augmented Rise of Angiotensin II During Exercise. J Am Coll Cardiol 52 (2008): 287-292.
- Sung KC, Hong YS, Lee JY, et al. Physical activity and the progression of coronary artery calcification. Heart 107 (2021): 1710-1716.
- Laddu DR, Rana JS, Murillo R, et al. 25-Year Physical Activity Trajectories and Development of Subclinical Coronary Artery Disease as Measured by Coronary Artery Calcium: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Mayo Clin Proc 92 (2017): 1660-1670.