The Impact of Cardiomyopathy on Patients' Daily Functioning
Wojciech Krzyzanowski1, Maciej Kusmierczyk*,2, Jakub Mlozniak2, Robert Morawiec3, Agata Tyminska2, Agata Galas4, Katarzyna Byczkowska5, Piotr Hamala6, Iwona Gorczyca-Glowacka7, Anna Furman-Niedziejko8, Dominika Klimczak-Tomaniak9, Agnieszka Major 10, Adrian Stefanski11, Witold Furmanek12, Marcin Grabowski2
1Cardiology Department, Masovian Specialist Hospital, Poland
21st Chair and Department of Cardiology, Medical University of Warsaw, Poland
32nd Department of Cardiology, Medical University of Lodz
4Department of Cardiology and Internal Diseases, Military Institute of Medicine,
Warsaw
5National Institute of Cardiology, Warsaw
61st Department and Chair of Cardiology, Medical University of Lodz
7Collegium Medicum, The Jan Kochanowski University, Kielce
8Department of Coronary Disease and Heart Failure, Institute of Cardiology, Jagiellonian University
Medical College, Krakow
9Department of Cardiology, Hypertension and Internal Medicine, Medical University of Warsaw
101st Clinic of Cardiology and Electrotherapy, Swietokrzyskie Cardiology Center, Kielce
11Department of Hypertension and Diabetology, Faculty of Medicine, Medical University of Gdansk
12Institute of Heart Diseases, Wroclaw Medical University
*Corresponding author: Maciej Kusmierczyk, 1st Chair and Department of Cardiology, Medical University of Warsaw, Poland.
Received: 19 April 2025; Accepted: 29 April 2025; Published: 22 July 2025
Article Information
Citation: Wojciech Krzyżanowski, Maciej Kuśmierczyk, Jakub Młoźniak, Robert Morawiec, Agata Tymińska, Agata Galas, Katarzyna Byczkowska, Piotr Hamala, Iwona Gorczyca- Głowacka, Anna Furman-Niedziejko, Dominika Klimczak-Tomaniak, Agnieszka Major, Adrian Stefański, Witold Furmanek, Marcin Grabowski. The Impact of Cardiomyopathy on Patients' Daily Functioning. Fortune Journal of Health Sciences. 8 (2025): 710-715.
Share at FacebookAbstract
Cardiomyopathy is a disease leading to heart failure, and consequently, to a deterioration in the quality of life of patients. Scales such as VAS and KCCQ-12 can facilitate proper management of patients diagnosed with this disease. In our study, we analyzed 398 patients selected from the HEROES cohort. This database was created thanks to the cooperation of specialist centers in Poland and allowed for the division of patients based on many factors, such as etiology, the scale of discomfort or problems with physical activity. In almost half of the patients (47.74%), the factor causing the disease could not be determined. The most common type of cardiomyopathy diagnosed was arrhythmic cardiomyopathy (38.44%). Patients were analyzed and grouped according to their quality of life and perceived pain and discomfort on the VAS and KCCQ-12 scales. We then compared the results according to the etiology of the disease. Our studies showed the need to deepen diagnostic methods in cardiomyopathy, especially in infectious cardiomyopathy and hereditary cardiomyopathy. There is also a need for further research on the widespread arrhythmic cardiomyopathy in order to understand its progressive progression and optimize the procedure in its treatment. Both scales we used proved to be helpful in analysis of the patients' condition and can be used to provide them with efficient help, for example in the psychological aspect. In the treatment of patients with cardiomyopathy, it is worth paying attention to improving the quality of life of patients and striving to reduce the symptoms associated with the disease.
Keywords
cardiomyopathy, heart failure, HEROES, KCCQ-12, VAS scale, quality of life
cardiomyopathy articles, heart failure articles, HEROES articles, KCCQ-12 articles, VAS scale articles, quality of life articles.
Article Details
Introduction
Cardiomyopathies are diseases of the heart muscle that cause changes in its functioning. They can occur as primary conditions (related to heart muscle disease) or secondary (resulting from multisystem diseases) [1]. Currently, they are more often classified based on morphological and functional phenotypes [2]. The most common primary cardiomyopathy is hypertrophic cardiomyopathy. Dilated cardiomyopathy develops due to genetic or acquired causes and presents with features of heart failure. Multisystem diseases may be accompanied by restrictive cardiomyopathy. The most common factors contributing to the disease include genetic factors, arrhythmias, infections, toxins (alcohol, medications, drugs), or diseases such as Chagas disease or Takotsubo syndrome [1]. In our study, we aimed to assess the quality of life in patients with cardiomyopathy. To properly evaluate this, we used, among other tools, the KCCQ (Kansas City Cardiomyopathy Questionnaire). The KCCQ scale is designed to easily assess all relevant health areas of patients, taking into account differences between men and women, younger and older patients, as well as those with different socio-economic statuses. The results are presented on a scale from 0 to 100, where lower scores indicate more severe symptoms or greater limitations, and 100 represents no symptoms, no limitations, and good quality of life [3]. More specifically, in our study, we used the shorter version of the scale, KCCQ-12. During the study, patients filled out a questionnaire assessing their quality of life. The questionnaire covered physical limitations, symptom frequency, quality of life, and social limitations. By converting the responses into scores using specific formulas, we were able to accurately evaluate the patients' daily functioning. In our study, we aim to highlight the impact of cardiomyopathy on patients' quality of life and compare our patient database with cohorts from other centers worldwide.
Methodology
This is a prospective, multi-center observational study aimed at presenting the health status of patients with heart failure (HF) based on a representative national sample. The study design and selection of centers were based on the long-term registry of HF patients, endorsed by the European Society of Cardiology and 25 national cardiology societies, including the Polish Cardiac Society.
The centers applying for participation in HEROES were evaluated based on geographical representation and equipment, following the guidelines of the EURObservational Research Program ESC:
- • representing all regions of Poland;
- • ensuring diversity in terms of specialized equipment: 25% of centers with cardiac surgery, 25% with a hemodynamics laboratory, and 50% without these facilities;
- • agreeing to provide full clinical data.
A total of 41 centers participated in the HEROES program, including 32% with cardiac surgery, 22% with a hemodynamics laboratory, and 46% without these facilities.
To ensure systematic patient enrollment, the registration process was conducted once a week. The eCRF, developed by the Scientific Committee, was accompanied by an investigator's brochure outlining the necessary procedures and definitions. The collected patient data complied with personal data protection regulations (including GDPR). The form was used to collect comprehensive clinical data, with its content depending on the available diagnostic and therapeutic tests. No additional examinations or treatments were required, except those resulting from the physician's decisions. Patients provided informed consent to participate, and data were updated during hospitalization. The analysis of the patient's condition was based on data from outpatient or hospital sources. The project started on April 2, 2022, and patient enrollment was completed by March 27, 2024, providing clinical and survival data for 1,422 patients (0% data loss). The average follow-up period was 16 months (median: 485 days, interquartile range: 397–599 days) [4]. For our study, we selected 398 patients who had been hospitalized for cardiomyopathy from the database and analyzed data on their quality of life, including physical limitations, symptom frequency, quality of life, and social limitations. Among other tools, we used specific scales such as the KCCQ-12 and the visual analogue scale (VAS).
Results
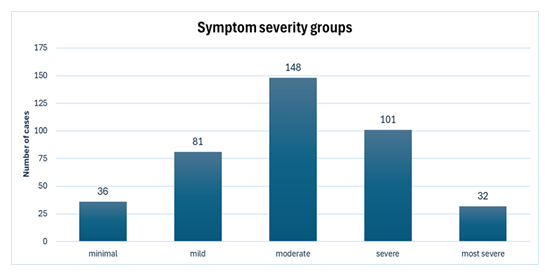
In the cohort of 398 patients, n=289, 73% male and n=109, 27% female, with average age of 63, arrhythmic cardiomyopathy was diagnosed in 153 patients (38.44%), infectious cardiomyopathy in 13 patients (3.27%), inherited genetic cardiomyopathy in 5 patients (1.26%), and drug-induced cardiomyopathy in 8 patients (2.01%), including 5 cases associated with anthracycline use and 3 cases where the etiology remained undetermined. Additionally, 28 patients (7.03%) were suspected to have toxic cardiomyopathy, with 24 cases linked to alcohol abuse, and 4 cases associated with cocaine use. Lastly, 1 patient (0.25%) had cardiomyopathy resulting from radiotherapy. The cause of cardiomyopathy could not be determined in 190 patients (47.74%). The first aspect we analyzed is the scoring of our patients on the Visual Analogue Scale (VAS). This scale assesses patients with a score ranging from 0 to 100, depending on the pain, discomfort, and other symptoms experienced [5]. We divided a cohort of 398 patients into groups based on the severity of the symptoms they experienced. The first group included 36 patients (9.05%) who rated their symptoms as minimal on the VAS scale (0-20 points). Mild discomfort (21–40 points) was reported by 81 patients (20.36%). The group with moderate symptoms (41-60) included 148 individuals (37.19%). Severe pain (61-80) was experienced by 101 patients (25.38%) and the most severe symptoms (81–100 points) were reported by 32 patients (8.04%). The results are shown in [Fig. 1]
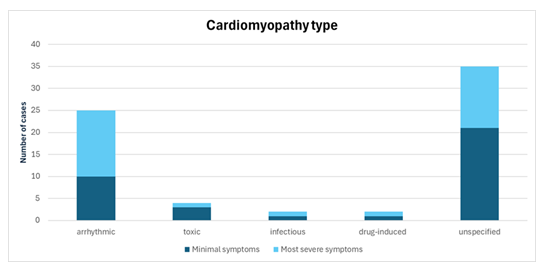
Next, based on the VAS scale, we analyzed the extreme scoring results. The first group included patients with minimal reported discomfort (0–20 points on the scale), while the second group comprised those experiencing the most severe symptoms (81–100 points). Among the 36 patients in Group 1, 10 (27.78%) had arrhythmic cardiomyopathy, three (8.33%) had toxic cardiomyopathy (all caused by alcohol abuse), one had infectious cardiomyopathy (2.78%), and one had drug-induced cardiomyopathy (2.78%). In 21 patients (58.33%), the etiology of the disease was unclear. The number of patients classified in the second group was 32. Among them, 15 (46.88%) had arrhythmic cardiomyopathy, while one patient each had infectious (3.13%), drug-induced (3.13%), and toxic cardiomyopathy (3.13%). In 14 patients (43.76%), the cardiomyopathy was of unknown origin. The results are shown in [Fig. 2].
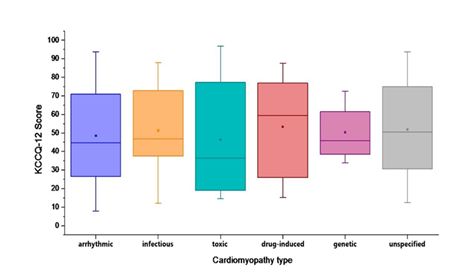
The most important asset of patients' quality of life in the study was the analysis of responses given on the abbreviated version of the KCCQ questionnaire (a scale dedicated to the assessment of patients' health and life in cardiomyopathy heart failure), the KCCQ-12. The questionnaire conducted questions focused on four aspects from patients' daily lives in the past 2 weeks. These included physical limitation, symptom frequency, quality of life and social limitation. The scores were scaled from 0 to 100, with 0 being the lowest reported health status and 100 being the highest.
In the study, various types of cardiomyopathies showed distinct patterns in patient-reported outcomes. For arrhythmic cardiomyopathy, patients reported moderate scores across physical limitation (48.75), symptom frequency (51.92), quality of life (42.89), and social limitation (51.72), with a total mean score of 48.82. Conversely, patients with unspecified cardiomyopathy experienced slightly higher scores in physical limitation (55.02), symptom frequency (61.99), quality of life (47.14), and social limitation (53.14), resulting in a total mean score of 54.32. Patients with infectious cardiomyopathy reported significant symptom frequency (71.15) compared to other groups, alongside moderate scores in physical limitation (53.69), quality of life (34.62), and social limitation (45.14), leading to a total mean score of 51.15. Meanwhile, those with hereditary cardiomyopathy indicated lower physical limitation (41.67) and quality of life (35.00) scores, despite higher symptom frequency (75.00) and social limitation (50.00), resulting in a total mean score of 50.42. Pharmacotherapy-induced cardiomyopathy exhibited higher scores in physical limitation (54.91) and symptom frequency (56.77), with moderate scores in quality of life (45.31) and social limitation (51.19), yielding a total mean score of 52.05. Radiotherapy-induced cardiomyopathy showed notably high physical limitation (66.67) but lower scores in symptom frequency (35.42), quality of life (37.5), and social limitation (33.33), with a total mean score of 43.23. Lastly, patients with toxic cardiomyopathy reported moderate scores across physical limitation (47.92), symptom frequency (50.74), quality of life (42.86), and social limitation (43.66), resulting in a total mean score of 46.29. The combined results are shown in [Fig. 3]. The middle line represents the median, and the dot represents the arithmetic mean. The bottom and top edges of the box correspond to the first (Q1) and third quartile (Q3), respectively. Whiskers cover a range of 5-95% of the data to eliminate outliers and better illustrate the central tendency of the results.
In the analysis of the individual components of the questionnaire, for daily activity, the biggest problem was the intensity of physical activity (n=176, 44% of patients showed extreme limitation), and the smallest was a basic activity like showering/bathing (n=162, 41% of patients have no problem with this activity). Most patients reported no swelling (n=156, 39%). Fatigue occurring at least once a day (n=189, 47%) as well as daytime dyspnea (n=170, 43%) were frequently reported symptoms. Nocturnal dyspnea was never present in most patients (n=222, 56%). The vast majority felt that cardiomyopathy had affected their enjoyment of life to some degree (n=250, 63%), with many patients (n=214, 54%) indicating an anticipated lack of satisfaction with life in the future. At the current stage of life, patients mention a perceived impact in matters of pursuing their hobbies (n=245, 62%) or the quality of their professional work (n=253, 64%).
Discussion
Firstly, our study provides information about the distribution of cardiomyopathy etiologies. Analyzing our results based on the etiology of cardiomyopathy, we observe difficulties in identifying the causative factor of the disease. In nearly half of the cases, the diagnosis was made without a clear indication of the underlying cause. The majority of patients with specific diagnosis (38,44%) were diagnosed with arrythmia cardiomyopathy. This shows the scale of occurrence of arrhythmic cardiomyopathy, the occurrence of which may result from genetic predisposition or acquired factors affecting heart functioning [6, 7]. Infectious cardiomyopathy detected in 3.27% of patients shows a relatively low risk of infection in our cohort. The situation is similar in hereditary cardiomyopathy, occurring in 1.26% of respondents. This may suggest that the diagnosis has not been extended to include genetic tests or that this type of cardiomyopathy has been incorrectly classified, for example, to a large group of cardiomyopathies of unknown causes.
In the case of drug-induced cardiomyopathy (2.01%), the main inducing factor was anthracyclines, which coincides with the current state of knowledge regarding the cardiotoxic effects of this group of drugs. [8] In three cases, it was not possible to determine the specific drug responsible for causing the disease, which shows the difficulties in correctly identifying the agent in this type of cardiomyopathy.
A large group of respondents (7.03%) were patients with diagnosed cardiomyopathy of toxic origin. Particularly noteworthy is the fact that out of 28 patients, 24 were caused by alcohol abuse, which confirms the destructive effect of chronic alcohol consumption on myocardial dysfunction. [9] The harmful effects of cocaine use have been documented in four cases, which also confirms the current state of knowledge about the substance [10]. The study included one case (0.25%) of cardiomyopathy as a complication after radiotherapy. This is a rare case but has been described as one of the late chest irradiations in oncology patients [11]. In our study, we categorized a cohort of 398 patients into a specific group based on the pain and discomfort they experienced. Most patients (37.19%) experienced moderate discomfort. We subjected extreme groups to special analysis. Comparing them, it can be seen that there are more patients with unclear origin of cardiomyopathy in the group experiencing minimal symptoms of discomfort (58.33% to 43.76% in group 2). This may be associated with scanty symptoms of the disease, which make it more difficult to determine the etiology of the disease or not enough time during hospitalization, required to specify the etiology of the disease. The most visible difference when comparing both groups can be seen in the case of arrhythmic cardiomyopathy (27.78% in group 1, 46.88% in group 2). There may be more patients experiencing significant discomfort due to the progressive nature of changes in arrhythmic cardiomyopathy. During episodes of the disease, additional symptoms may appear, such as exercise intolerance, heart palpitations and dizziness. These symptoms may influence the final VAS score, increasing the score. [6, 7]
There were more patients with toxic cardiomyopathy in group 1 (8.33% vs. 3.13% in group 2). This may be due to the slower development of alcohol-induced cardiomyopathy. The disease develops over a longer period of time and may not cause severe symptoms or severe discomfort [9]. There was no difference in the number of patients with drug-induced and infectious cardiomyopathy. These results may indicate a different clinical picture of both cardiomyopathies, where symptoms vary depending on the stage of the disease, involvement of the heart muscle and individual variability. The KCCQ-12 scale used in the study was a valid exponent for assessing patients' quality of life. Its high reliability, high correlation, and comparable prognostic and clinical interpretation when compared with its full version, the KCCQ scale, have been repeatedly demonstrated [13]. The number of procedures, tests and possible scales performed is numerous, hence the need to streamline and shorten single visits. Fortunately, these scales can be used interchangeably to improve physician workflow without sacrificing treatment quality [15]. The benefits of using the scale also carry over to physician-patient interaction. It serves as a helpful tool for collecting patient history, improving conversation and tracking progress in therapy, providing greater satisfaction with the services received. [14] Better relations induce better monitoring of patient’s health status through various visits. Despite establishing a closer relationship with the patient, regular administration of the questionnaire does not affect decision-making in the treatment process.
The profile of cardiomyopathy patients in this study and similar analyses points out to rather elder individuals. The effectiveness of the KCCQ-12 scale has also been proven among a highly elderly population. [12] Among them, low scale exponents coincide with poor quality of life, worse NYHA score and other laboratory exponents and patient assessment scales. Low scale scores also show higher mortality and overall hospitalizations rates. Equally important factor is no improvement after a one-year follow-up, as it worsens the prognosis, especially in women. Of the 4 categories in the KCCQ-12 scale, the highest score was given to the frequency of symptoms presented, which indicates its general lack of severity. This may be due to the very nature of cardiomyopathy, which is a chronic degenerative process lasting many years. In its case, we are most concerned about exacerbation of the chronic condition and sudden deterioration of health, with the need for urgent. On the opposite side, quality of life received the lowest scores. Constantly accompanying symptoms when performing longer or more strenuous tasks are able to take away the patient's enjoyment of any activity, leading to lowered mood and the development of depressive disorders. Sometimes the need to implement psychological support is a usually forgotten element of patient therapy. A positive effect on KCCQ-12 scale scores after 30 days has been demonstrated in patients with self-coaching implemented after hospitalization. [16] It was also associated with a reduction in the frequency of symptoms reported by patients.
Conclusions
Our work illustrates the impact of cardiomyopathy on the quality of life of patients, taking into account its etiology and accompanying symptoms. The first conclusion visible in the research is the need to expand diagnostics and strive to facilitate finding the causes of the disease. This is especially important in the case of infectious and hereditary cardiomyopathies, which can be the cause of the disease with a great deal of certainty in cases that are difficult to determine. Among the identified etiologies of cardiomyopathy in our study, we came across a large number of cases of arrhythmic cardiomyopathy. This may indicate the need for further research on this type of cardiomyopathy. This is also confirmed by the analysis of patients on the VAS scale, which illustrated the progressive nature of changes in this type. Another aspect of our research was the visualization of the patients' condition using the KCCQ-12 scale. Thanks to it, the quality of life of patients can be assessed quickly and precisely. In the case of patients with low scores, there may be a significant mental burden and a decrease in the quality of life. In such situations, we can recommend psychological consultations to patients, resulting in an improvement in their condition. In summary, cardiomyopathy research should focus on improving the precision of disease diagnostics. Genetic testing, for example, can be helpful in this aspect [17]. Additionally, diagnostic aids in the form of the VAS or KCCQ-12 scale are very useful in quickly and accurately assessing the patient's condition, which makes it possible to provide specialist care tailored to the individual needs of the patient.
Declarations
Ethics approval and consent to participate: HEROES was approved by Bioethical Committee in Medical University of Lodz (decision number: RNN/316/20/KE from 20th Dec 2020, update: KE/762/23 from 12th Sep 2023).
Consent for publication: Not Applicable
Availability of data and materials: All the data sets used are included in the published article.
Competing interests: All authors have no competing interests to declare
Funding: Polish Cardiac Society (Contract No. CRU 0120-KCKB-2023)
Dataset: Polskie Towarzystwo Kardiologiczne / Polish Cardiac Society. 2023. Badanie Obserwacyjne Niewydolnosci Serca Polskiego Towarzystwa Kardiologicznego / Heart Failure Observational Study (HEROES). Medical University of Lodz. https://doi.org/10.60941/JVH1-5190.
Authors' Contributions: K. W. - conceptualization, data curation, project administration, visualization, writing, supervision K. M. - conceptualization, data curation, project administration, visualization, writing, M. J. - conceptualization, data curation, project administration, visualization, writing, G. M. – supervision, M. R. - methodology, resources, investigation, G. A. - - methodology, resources, investigation, T. A. - methodology, resources, investigation, B. K. - methodology, resources, investigation, F-N. A. - methodology, resources, investigation, T. M. - methodology, resources, investigation, S. A. - methodology, resources, investigation, M. A. - methodology, resources, investigation, K-T. D. - methodology, resources, investigation, H. P. - methodology, resources, investigation, Z. M. - methodology, resources, investigation, G-G. I. - methodology, resources, investigation, S. M. - methodology, resources, investigation, N. M. - methodology, resources, investigation.
Acknowledgements: Not applicable
Authors' information: Not applicable
References
- Brieler J, Breeden MA, Tucker J. Cardiomyopathy: An Overview. Am Fam Physician 96 (2017): 640-646.
- McKenna WJ, Marron BJ, Thiene G. Classification, Epidemiology, and Global Burden of Cardiomyopathies. Circulation Research 121 (2017): 722-730.
- John A. Spertus, Philip G. Jones, Alexander T. Sandhu, et al, Interpreting the Kansas City Cardiomyopathy Questionnaire in Clinical Trials and Clinical Care: JACC State-of-the-Art Review, Journal of the American College of Cardiology 76 (2020): 2379-2390.
- Drózdz J, Morawiec R, Drozd M, et al, Rationale, objectives and design of the Heart Failure Observational Study of the Polish Cardiac Society (HEROES), Polish Heart Journal (Kardiologia Polska) (2024): 1897-4279.
- Sung YT, Wu JS. The Visual Analogue Scale for Rating, Ranking and Paired-Comparison (VAS-RRP): A new technique for psychological measurement. Behav Res 50 (2018): 1694–1715.
- Shoureshi P, Tan AY, Koneru J, et al, Arrhythmia-Induced Cardiomyopathy: JACC State-of-the-Art Review, Journal of the American College of Cardiology 83 (2024): 2214-2232.
- Desai, Dev MD, Maheta, Darshil kumar MD, et al. Understanding Arrhythmia-Induced Cardiomyopathy: Symptoms and Treatments. Cardiology in Review (2024).
- Keith Dadson, Oscar Calvillo-Argüelles, Paaladinesh Thavendiranathan, et al. Anthracycline-induced cardiomyopathy: cellular and molecular mechanisms. Clin Sci (Lond) 17 July 134 (2020): 1859–1885.
- Fernando Domínguez, Eric Adler, Pablo García-Pavía, Alcoholic cardiomyopathy: an update, European Heart Journal 45 (2024): 2294–2305.
- Arenas DJ, Beltran S, Zhou S, et al. Cocaine, cardiomyopathy, and heart failure: a systematic review and meta-analysis. Sci Rep 10 (2020): 19795.
- Thalambedu N, Khan Y. Fluorouracil (5-FU)-induced Cardiomyopathy. Cureus 11 (2019): e5162.
- Luiso D, Herrero-Torrus M, Badosa N, et al. Quality of Life in Older Patients after a Heart Failure Hospitalization: Results from the SENECOR Study. J Clin Med 11 (2022): 3035.
- Spertus JA, Jones PG. Development and Validation of a Short Version of the Kansas City Cardiomyopathy Questionnaire. Circ Cardiovasc Qual Outcomes 8 (2015): 469-76.
- Brown-Johnson C, Calma J, Amano A, et al. Evaluating the Implementation of Patient-Reported Outcomes in Heart Failure Clinic: A Qualitative Assessment. Circ Cardiovasc Qual Outcomes 16 (2023): e009677.
- Sauer AJ, Sherrod CF, Gosch KL, et al. The Psychometric Performance of the Kansas City Cardiomyopathy Questionnaire-12 in Symptomatic Obstructive Hypertrophic Cardiomyopathy. J Card Fail 28 (2024): S1071-9164(24)00417-2.
- Stubblefield WB, Jenkins CA, Liu D, et al. Improvement in Kansas City Cardiomyopathy Questionnaire Scores After a Self-Care Intervention in Patients with Acute Heart Failure Discharged from the Emergency Department. Circ Cardiovasc Qual Outcomes 14 (2021): e007956.
- Chiswell K, Zaininger L, Semsarian C, Evolution of genetic testing and gene therapy in hypertrophic cardiomyopathy, Progress in Cardiovascular Diseases 80 (2023): 38-45.