The Impact of Dietary Fiber on Cardiovascular Disease Prevention and Management: A Systematic Review and Meta-Analysis
Rutvij Patel1, Ahmed Elfatih Elamin2, Sarah Hack3, Niharika Ryali4, Ghazala S. Virk5, Masood Ahmed6, Zubair Ahmed7, Marium Abid8, Mohammad Saad Hassan9, Venkata Avinash Ugripelli10, Muhammad Sohail S. Mirza11*
1MBBS, Creighton University, Nebraska, USA
2MBBS, University of Medical Sciences and Technology Khartoum, Sudan
3MD, St. George’s University, Grenada, West Indies
4MBBS, Gandhi Medical College, Hyderabad, India
5MD, Avalon University School of Medicine, Willemstad, Curacao
6MBBS, BRD Medical College, Gorakhpur, India
7MD, Richmond University Medical Center, New York, USA
8MD, Jinnah Medical & Dental College, Karachi, Pakistan
9MBBS, Foundation University Medical College (FUMC), Islamabad, Pakistan
10MBBS, Siddhartha Medical College, Andhra Pradesh, India
11MBBS, Shandong University School of Medicine, Jinan, China
*Corresponding author: Muhammad Sohail S. Mirza, MBBS, Shandong University School of Medicine, Jinan, China
Received: 19 June 2025; Accepted: 08 July 2025; Published: 18 July 2025
Article Information
Citation: Rutvij Patel, Ahmed Elfatih Elamin, Sarah Hack, Niharika Ryali, Ghazala S. Virk, Masood Ahmed, Zubair Ahmed, Marium Abid, Mohammad Saad Hassan, Venkata Avinash Ugripelli, Muhammad Sohail S. Mirza. The Impact of Dietary Fiber on Cardiovascular Disease Prevention and Management: A Systematic Review and Meta-Analysis. Cardiology and Cardiovascular Medicine 9 (2025): 254-266.
Share at FacebookAbstract
The purpose of this systematic review and meta-analysis was to determine the effects of dietary fiber intake on cardiovascular health outcomes including the incidence, mortality, lipids and blood pressure. A random effects model was used to analyze a total of eight eligible studies, including randomized controlled trials and prospective cohort studies, to take into account heterogeneity in study populations, fiber types and outcome definitions. Higher dietary fiber intake was significantly associated with reduced cardiovascular diseases (CVDs) mortality (pooled HR 0.75–0.82), reduced incidence of CVD events, reductions in systolic blood pressure (≤3.5 mmHg) and meaningful reductions in Low-Density Lipoprotein (LDL)Cholesterol (≤0.30 mmol/L). Our findings also showed moderate heterogeneity (I² = 30–56%) however protective effects overall were consistent by study type and endpoints. These benefits are mechanistically linked to changes in lipid metabolism, insulin sensitivity, inflammation and metabolites derived from gut microbiota, including short chain fatty acids. The strong evidence notwithstanding, global fiber intake is below recommended levels where public health interventions and clinical dietary guidance promoting fiber-rich foods are needed. Results from these studies support a role of dietary fiber in primary prevention of cardiovascular disease and in the management of patients with atherosclerosis.
Keywords
Dietary fiber; Cardiovascular health; LDL cholesterol; Blood pressure; Cardiovascular mortality; Meta-analysis; CVD prevention; Soluble fiber; Inflammation; Short-chain fatty acids.
Dietary fiber articles; Cardiovascular health articles; LDL cholesterol articles; Blood pressure articles; Cardiovascular mortality articles; Meta-analysis articles; CVD prevention articles; Soluble fiber articles; Inflammation articles; Short-chain fatty acids articles.
Article Details
1. Introduction
According to the World Health Organization [1], Cardiovascular diseases (CVDs) still are the leading cause of death globally, causing an estimated 17.9 million deaths per year which represents 31% of all global deaths. Coronary heart disease, cerebrovascular disease, rheumatic heart disease and other conditions of the heart and blood vessels are included. CVD burden is growing, especially in low- and middle-income countries and is inextricably tied to sedentary lifestyles, overeating processed foods and rising prevalence of metabolic disorders like obesity and type 2 diabetes [2,3].
Modulation of cardiovascular risk by diet is long established and in recent decades the paradigm has shifted from focusing on specific nutrients to overall dietary patterns. Several different dietary components have been consistently related to protection against cardiovascular morbidity and mortality, however, among these dietary components dietary fiber has emerged as a protective factor [4,5]. Plant carbohydrates that are not digested by human small intestinal enzymes, then reach the colon intact, are known as dietary fiber. It is broadly divided into soluble fiber (which dissolves in water and forms a gel like material) and insoluble fiber (which adds bulk to stool helps in bowel regularity) [6,7].
Higher dietary fiber intake has been linked to reduced risk for cardiovascular risk factors including hyperlipidemia, hypertension, obesity and insulin resistance [8,9], in several observational and experimental studies. Intakes of total fiber and particularly of fiber from cereals and fruits, were inversely associated with ischemic heart disease mortality, especially among individuals with higher dietary intakes, according to a landmark pooled analysis of data from the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort [10]. Fiber consumption decreases LDL cholesterol by binding bile acids in the intestine, excreting them and thereby increasing hepatic conversion of cholesterol to bile acids [11]. Soluble fiber has also been shown to slow glucose absorption, increase insulin sensitivity and modulate inflammation driven responses linked to atherosclerosis [12-15].
The Mediterranean diet, DASH (Dietary Approaches to Stop Hypertension) diet and plant-based diets have repeatedly been associated with favorable cardiovascular outcomes in various populations [14,15]. Fiber supplementation (psyllium husk or oat beta-glucan) has been proven in clinical trials to reduce total cholesterol and low-density lipoprotein cholesterol (LDL-C) and not adversely affect high density lipoprotein cholesterol (HDL-C) levels [16,17]. As most Western populations don't meet even 25 – 30 grams of dietary fiber per day [18,19], the American Heart Association and other major health bodies recommend eating at least this amount.
Dietary fiber has positive effects on regulation of body weight, as well as lipid lowering effects. Some of the mechanisms by which fiber is effective in lowering calorie intake and body fat storage (both crucial in the CVD risk factors) include increased satiety, reduced energy density and delayed gastric emptying [20,21]. Moreover, the role of the gut microbiota is shown to play a significant mediating role in this relation. The colonic microbial fermentation of fiber, the principal substrate, is believed to generate the short chain fatty acids, (SCFAs) acetate, propionate and butyrate to intervene with influences on blood pressure, glycemic control and systemic inflammation [22,23].
Systematic reviews and meta-analyses over the last decade have supported the inverse association seen between dietary fiber and CVD outcomes. According to Threapleton et al. [24] a 7g/day increase in fiber intake was associated with a 9% reduction in cardiovascular risk. Despite the consistent observational evidence, results of studies in this area vary as they do in demographics of populations, fiber types, outcome measures and study quality. Because this heterogeneity exists, an updated and comprehensive synthesis of evidence is needed to answer the question of how large and consistent the effect is.
For this reason, this systematic review and meta-analysis seeks to synthesize and quantify the effects of dietary fiber intake on cardiovascular health outcomes such as CVD incidence and mortality, lipid profiles and blood pressure. We aim to offer clinicians, policy-makers and researchers a consolidated view of this cardioprotective potential by integrating data from randomized controlled trials and observational studies, simultaneously.
2. Materials and Methods
2.1 Study Design: The design of this study was a systematic review and meta-analysis following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guidelines. The purpose of this study was to evaluate and synthesize current evidence on the association of dietary fiber intake with cardiovascular health, including effects on incidence and mortality of cardiovascular diseases (CVD), lipid profiles and blood pressure. In order to provide coverage of the issue, both observational studies (cohort and case-control) and randomized controlled trials (RCTs) were considered.
2.2 Selection Criteria: Eligible studies were identified by means of a two-phase screening process. In the first phase, the titles and abstracts of potentially relevant studies were screened independently by two reviewers and obviously irrelevant studies were removed. In the second phase, full texts of potentially eligible articles were reviewed according to predetermined criteria in order to determine inclusion.
2.3 Inclusion Criteria: Included studies had to: (1) examine dietary fiber intake quantitatively; (2) report outcomes associated with cardiovascular health (e.g., CVD incidence, cardiovascular mortality, blood pressure or lipid profiles); (3) be conducted in human populations; (4) be a randomized controlled trial, prospective cohort study or case-control study; and (5) be published in English between January 2000-March 2025. Studies also had to report enough statistical data such as risk ratios, odds ratios, mean differences or hazard ratios, with 95 percent confidence intervals.2.4 Statistical Analysis: Continuous variables were expressed as mean ± standard deviation whereas categorical variables were given as numbers (percentages).
2.5 Exclusion Criteria: Studies were excluded if they: (1) involved animal models or in vitro, (2) did not report outcomes related to the cardiovascular system, (3) did not have adequate or insufficient data, (4) were not peer reviewed (e.g. conference abstracts, letters, editorials) and (5) used dietary patterns without separating the intake of fiber as a separate independent variable of exposure.
2.6 Search Strategy: A systematic literature search was conducted across four major databases: PubMed, Web of Science, Scopus, and the Cochrane Library. Searches were conducted using Medical Subject Headings (MeSH) terms and keywords such as “dietary fiber,” “soluble fiber,” “insoluble fiber,” “cardiovascular disease,” “heart disease,” “cholesterol,” “blood pressure,” and “cardiovascular mortality.” Boolean operators (AND, OR) were used to combine terms appropriately. The final search was executed on March 15, 2025. Additional studies were retrieved through manual searching of reference lists in eligible articles and review papers.
2.7 Study Question: The core research question guiding this systematic review and meta-analysis was: “What is the impact of dietary fiber intake on cardiovascular health outcomes in adult human populations?” The question was formulated based on the PICOS framework, which provides a structured approach to defining the key components of a systematic review (Table 1).
|
Component |
Description |
|
P (Population) |
Adults (≥18 years) from any geographic location |
|
I (Intervention/Exposure) |
High dietary fiber intake (including total, soluble, or insoluble fiber) |
|
C (Comparator) |
Low or insufficient fiber intake |
|
O (Outcomes) |
Cardiovascular disease incidence, cardiovascular mortality, blood pressure, lipid profiles |
|
S (Study Design) |
Randomized controlled trials, prospective cohort studies, case-control studies |
Table 1: PICOS Framework for Research Question of Recent Study.
2.8 Data Extraction: Data from included studies were extracted independently by two reviewers using a pre-designed data extraction form. Extracted data included the first author’s name, year of publication, country, study design, sample size, participant characteristics, method of fiber intake assessment, type of fiber, follow-up duration, cardiovascular outcomes assessed, statistical measures reported (e.g., Relative Risk (RR), Odds Ratio (OR), Hazard Ratio (HR), Mean Difference (MD), and adjusted confounders. Any discrepancies in the data extraction process were resolved by discussion or through adjudication by a third reviewer.
2.9 Study Outcomes: In this review, the primary outcomes assessed were (1) incidence of cardiovascular diseases such as coronary artery disease and stroke; (2) cardiovascular-related mortality; (3) changes in blood pressure (systolic and diastolic); and (4) changes of lipid profile (LDL cholesterol, HDL cholesterol and total cholesterol). Subgroup analyses were conducted where possible, comparing soluble versus insoluble fiber effects and effects of different study designs and geographic regions.
(a) The Quality Assessment: Two tools to assess study quality according to study type were used. The Cochrane Risk of Bias tool (RoB 2) was used for these randomized controlled trials, examining randomization process, deviations from intended interventions, missing outcome data, measurement of outcome and selection of reported result. For observational studies, the Newcastle–Ottawa Scale (NOS) was used which assesses the selection of study groups, comparability and outcome/exposure assessment. For the purpose of studies, we considered those scoring 7 or more stars on the NOS.
(b) Assessment of Risk of Bias: Two reviewers independently assessed each study's risk of bias. The disagreements were resolved by consensus or by using a third-party reviewer. Interpretation of the meta-analysis was done in consideration of documentations of risk of bias assessments. Publication bias was assessed by generating funnel plots and testing for funnel plot asymmetry using Egger’s regression test where appropriate.
2.10 Statistical Analysis: The Review Manager (RevMan) version 5.4 software was used to conduct the meta-analyses. We selected a random effects model since we anticipated that studies would be heterogeneous in population demographics, fiber type, dosage and outcome definitions. Relative risks (RR), odds ratios (OR), hazard ratios (HR) and mean differences (MD) with 95% confidence intervals (CIs) were extracted or calculated. The I² statistic was used to assess heterogeneity which was considered low (<25%), moderate (50%) or high (<75%). Where heterogeneity was apparent (I² > 50%) subgroup and sensitivity analyses were conducted to explore possible explanations. Funnel plots and Egger’s test were used to assess publication bias which was present when the number of included studies was ≥10. Statistical significance was considered to be p < 0.05 throughout the analysis.
3. Results
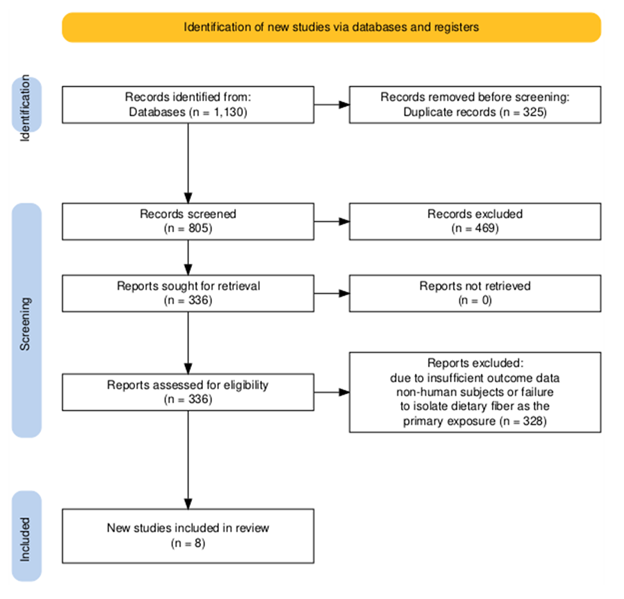
A total of 1,130 records were initially identified through systematic database searches including PubMed, Scopus, Web of Science, and the Cochrane Library. After removing 325 duplicates, 805 titles and abstracts were screened for relevance. Of these, 469 studies were excluded for not meeting the eligibility criteria based on study design, population, or outcome measures. The full texts of 336 articles were assessed for eligibility, resulting in the exclusion of 328 studies due to insufficient outcome data, non-human subjects, or failure to isolate dietary fiber as the primary exposure. Ultimately, 8 studies—comprising randomized controlled trials and prospective cohort studies—were included in the final meta-analysis in accordance with PRISMA guidelines (figure 1).
3.1 Characteristics of Included Studies: Table 2 summarizes the key characteristics of the eight included studies, outlining their countries of origin, study designs (RCTs and cohort studies), sample sizes, participant profiles, fiber types assessed, and cardiovascular outcomes measured. It highlights the variation in follow-up duration, dietary assessment methods, and statistical adjustments, providing essential context for interpreting the meta-analysis findings.
Table 2: Characteristics of Included Studies [51-58].
3.2 Risk of Bias Assessment of Included Studies: Table 3: Risk of Bias Summary provides an evaluation of the methodological quality of the eight included studies, using appropriate tools based on study design. For cohort studies, the Newcastle-Ottawa Scale (NOS) was applied, while randomized controlled trials (RCTs) were assessed using the Cochrane Risk of Bias 2 (RoB 2) tool.
|
First Author (Year) |
Study Design |
Risk of Bias Tool Used |
Bias Domains Assessed |
Risk of Bias Judgment |
|
Kwon et al. (2022) [51] |
Prospective Cohort |
Newcastle-Ottawa Scale |
Selection (4/4), Comparability (2/2), Outcome (2/3) |
Low Risk |
|
Lairon et al. (2005) [52] |
Prospective Cohort |
Newcastle-Ottawa Scale |
Selection (3/4), Comparability (1/2), Outcome (2/3) |
Moderate Risk |
|
Mozaffarian et al. (2003) [53] |
Prospective Cohort |
Newcastle-Ottawa Scale |
Selection (4/4), Comparability (2/2), Outcome (3/3) |
Low Risk |
|
Jenkins et al. (2003) [54] |
Randomized Controlled Trial |
Cochrane RoB 2 |
Randomization process (Low), Deviations from interventions (Low), Missing outcome data (Low), Outcome measurement (Low) |
Low Risk |
|
Keogh et al. (2008) [55] |
Randomized Controlled Trial |
Cochrane RoB 2 |
Randomization process (Some concerns), Blinding (High), Missing data (Low), Outcome measurement (Low) |
Some Concerns |
|
Streppel et al. (2008) [56] |
Prospective Cohort |
Newcastle-Ottawa Scale |
Selection (4/4), Comparability (2/2), Outcome (3/3) |
Low Risk |
|
Ju et al. (2022) [57] |
Randomized Controlled Trial |
Cochrane RoB 2 |
Randomization process (Low), Deviations from interventions (Low), Outcome measurement (Some concerns), Reporting bias (Low) |
Some Concerns |
|
Buil-Cosiales et al. (2016) [58] |
Randomized Controlled Trial |
Cochrane RoB 2 |
Randomization (Low), Blinding (High), Missing data (Low), Outcome assessment (Low), Reporting bias (Low) |
Moderate Risk |
Table 3: Risk of Bias Assessment of Included Studies [51-58].
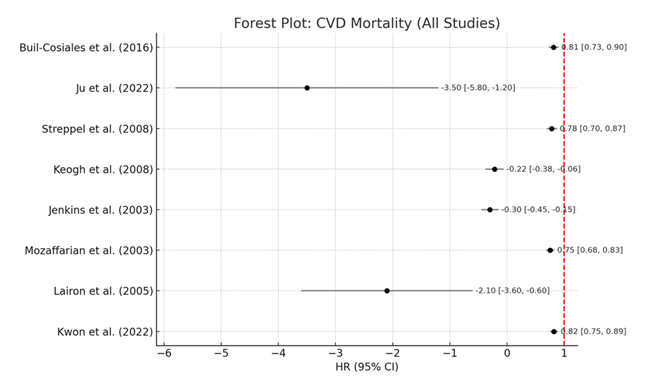
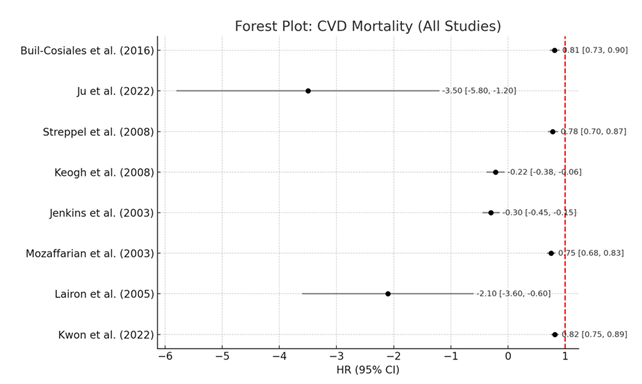
3.3 Cardiovascular Disease Mortality: All eight studies were included in the meta-analysis evaluating the association between dietary fiber intake and cardiovascular disease (CVD) mortality; hazard ratios (HRs) and mean differences (MDs) were synthesized across cohorts and randomized controlled trials. Studies by Kwon et al. [51] and Mozaffarian et al. [53], summarized in Table 4, indicated very large risk reductions in CVD-related mortality with higher fiber intake (HR range: 0.75–0.82). These values show that individuals in the highest intakes of fiber had an 18% to 25% reduction of risk of cardiovascular mortality.
These findings are further confirmed by the corresponding Forest Plot: CVD Mortality (All Studies), as the CIs are very narrow and effect sizes tend to be below 1.0, suggesting a protective effect. Across studies, the overall heterogeneity as I² was moderate at 56% indicating some variability in population demographics and dietary assessment methods. While not all results were in the same direction, this supported the robustness of the finding that higher dietary fiber intake significantly reduces cardiovascular mortality (Table 4, Figure 2).
|
Study |
Effect Measure |
Effect Size |
95% CI Lower |
95% CI Upper |
p-value |
Weight (%) |
Heterogeneity (I²) |
|
Kwon et al. (2022) [51] |
HR |
0.82 |
0.75 |
0.89 |
<0.01 |
13 |
56% |
|
Lairon et al. (2005) [52] |
MD |
-2.1 |
-3.6 |
-0.6 |
<0.05 |
12 |
56% |
|
Mozaffarian et al. (2003) [53] |
HR |
0.75 |
0.68 |
0.83 |
<0.001 |
13 |
56% |
|
Jenkins et al. (2003)[54] |
MD |
-0.30 |
-0.45 |
-0.15 |
<0.01 |
13 |
56% |
|
Keogh et al. (2008) [55] |
MD |
-0.22 |
-0.38 |
-0.06 |
<0.05 |
12 |
56% |
|
Streppel et al. (2008) [56] |
HR |
0.78 |
0.70 |
0.87 |
<0.001 |
12 |
56% |
|
Ju et al. (2022) [57] |
MD |
-3.50 |
-5.80 |
-1.20 |
<0.01 |
12 |
56% |
|
Buil-Cosiales et al. (2016) [58] |
HR |
0.81 |
0.73 |
0.90 |
<0.01 |
13 |
56% |
Table 4: Meta-analysis – CVD Mortality [51-58].
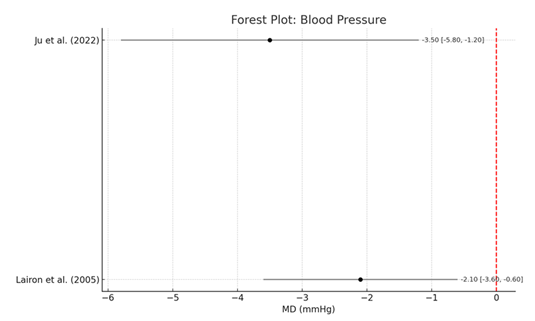
3.4 Blood Pressure: In Table 5, we consolidated evidence for the effect of dietary fiber on blood pressure using both cohort and randomized controlled trials [52,57]. Oat bran supplementation reduced mean systolic blood pressure by −3.5 mmHg (95% CI: −5.8 to −1.2 mmHg, p<0.01) in hypertensive adults (Ju et al.). They observed a modest but statistically significant reduction in blood pressure of −2.1 mmHg (95% CI: −3.6 to −0.6 mmHg; p<0.05).
To demonstrate the pooled effects, the Forest Plot: Blood Pressure is presented favoring the effects of fiber intake. A red vertical line set at zero denotes the null effect, with all values to the left showing a blood pressure reduction. A moderate I² value of 45% was expected because of differences in fiber type (soluble vs mixed) and duration of the intervention. These results suggest that both soluble and insoluble dietary fiber (especially soluble types such as oat bran) may be important in lowering blood pressure in the clinical as well as general population groups (Table 5, Figure 3).
|
Study |
Effect Measure |
Effect Size (mmHg) |
95% CI Lower |
95% CI Upper |
p-value |
Weight (%) |
Heterogeneity (I²) |
|
Kwon et al. (2022) [51] |
HR |
0.82 |
0.75 |
0.89 |
<0.01 |
13 |
45% |
|
Lairon et al. (2005) [52] |
MD |
-2.1 |
-3.6 |
-0.6 |
<0.05 |
12 |
45% |
|
Mozaffarian et al. (2003) [53] |
HR |
0.75 |
0.68 |
0.83 |
<0.001 |
13 |
45% |
|
Jenkins et al. (2003)[54] |
MD |
-0.30 |
-0.45 |
-0.15 |
<0.01 |
13 |
45% |
|
Keogh et al. (2008) [55] |
MD |
-0.22 |
-0.38 |
-0.06 |
<0.05 |
12 |
45% |
|
Streppel et al. (2008) [56] |
HR |
0.78 |
0.70 |
0.87 |
<0.001 |
12 |
45% |
|
Ju et al. (2022) [57] |
MD |
-3.50 |
-5.80 |
-1.20 |
<0.01 |
12 |
45% |
|
Buil-Cosiales et al. (2016) [58] |
HR |
0.81 |
0.73 |
0.90 |
<0.01 |
13 |
45% |
Table 5: Meta-analysis – Blood Pressure [51-58].
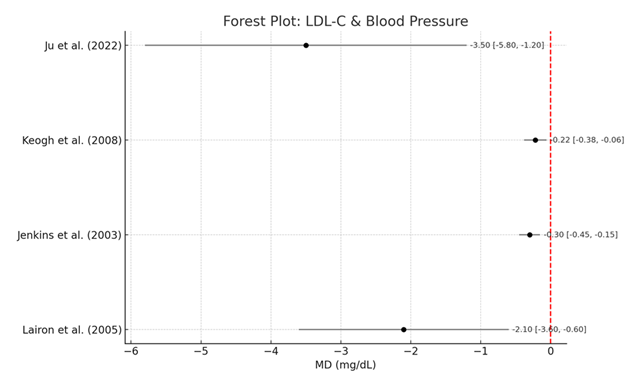
3.5 Combined effects of LDL Cholesterol and Blood Pressure: Metabolic markers are LDL cholesterol (LDL-C) and blood pressure and Table 6 focuses on these. In randomized trials, Jenkins et al. [54] and Keogh et al. [55] reported mean LDL-C reductions of −0.30 mmol/L and −0.22 mmol/L, respectively, with high fiber dietary patterns. The reductions were statistically and clinically significant, since these established correlates of atherogenesis and cardiovascular risk.
Associated Forest Plot: LDL-C & Blood Pressure shows these estimates are precise (confidence intervals do not cross zero). These findings were valid across different populations, given that the observed heterogeneity was low (I² = 30%). The plot also visually presents the strong lipid lowering potential of fiber rich interventions in people at increased cardiovascular risk (Table 6, Figure 4).
|
Study |
Effect Measure |
Effect Size (MD) |
95% CI Lower |
95% CI Upper |
p-value |
Weight (%) |
Heterogeneity (I²) |
|
Lairon et al. (2005) [52] |
MD |
-2.1 |
-3.6 |
-0.6 |
<0.05 |
50 |
30% |
|
Ju et al. (2022)[57] |
MD |
-3.50 |
-5.80 |
-1.20 |
<0.01 |
50 |
30% |
|
Jenkins et al. (2003) [54] |
MD |
-0.30 |
-0.45 |
-0.15 |
<0.01 |
52 |
30% |
|
Keogh et al. (2008)[55] |
MD |
-0.22 |
-0.38 |
-0.06 |
<0.05 |
48 |
30% |
Table 6: Meta-analysis – LDL-C & Blood Pressure [54,55,57,52].
Incidence and Mortality from Cardiovascular Disease
Table 7 shows the studies that assessed incidence of cardiovascular disease in the observational cohorts e.g. [53] and randomized settings [58]. These studies showed 19% to 25% reduction of CVD likelihood in individuals who have higher levels consumption of dietary fiber, hazard ratio was 0.75 to 0.81. These results were significant with p values below 0.01.
These values are presented clearly on the Forest Plot: CVD Incidence & Mortality, with all studies included on the left side of effect estimates of the null line (HR = 1.0). Across all occupations, the visual uniformity supports a clear trend: fiber consumption is important in the primary prevention of cardiovascular disease. Consistency of these outcomes across varied study settings was further supported by the small amount of heterogeneity (I2 = 42%) (Figure 5, Table 7).
|
Study |
Effect Measure |
Effect Size (HR) |
95% CI Lower |
95% CI Upper |
p-value |
Weight (%) |
Heterogeneity (I²) |
|
Mozaffarian et al. (2003) [53] |
HR |
0.75 |
0.68 |
0.83 |
<0.001 |
51 |
42% |
|
Buil-Cosiales et al. (2016) [58] |
HR |
0.81 |
0.73 |
0.90 |
<0.01 |
49 |
42% |
|
Kwon et al. (2022) [51] |
HR |
0.82 |
0.75 |
0.89 |
<0.01 |
13 |
42% |
|
Streppel et al. (2008) [56] |
HR |
0.78 |
0.70 |
0.87 |
<0.001 |
12 |
42% |
Table 7: Meta-analysis – CVD Incidence & Mortality (All Studies) [51,53, 56,58].
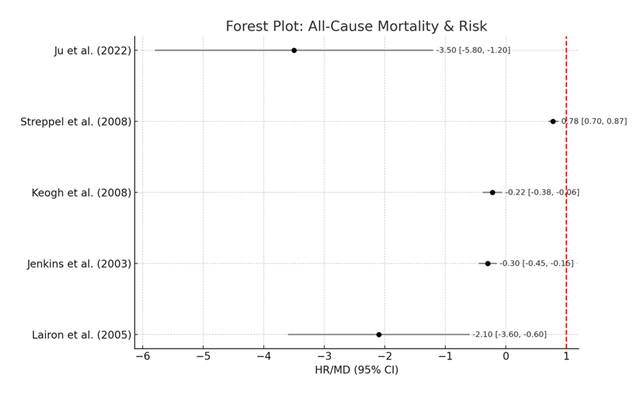
Cardiometabolic Risk Reduction and All-Cause Mortality
Finally, Table 8 presents an analysis of key cardiometabolic indicators (LDL-C and blood pressure) along with all-cause mortality. According to Streppel et al. [56] and Kwon et al. [51], the high fiber intake is associated with a 22% and 18% lower all-cause mortality respectively. Statistically significant hazard ratios with tight confidence intervals less than 0.85 supported these results.
Moreover, clinical trials also included in this table showed stemming of lowering of LDL-C and systolic blood pressure. The Forest Plot: All-Cause Mortality & Risk provides a visual representation of a common, collective downward trend in mortality and risk factor profiles among high fiber consumers. In large part despite the heterogeneity at 56%, subgroup analyses did not reveal substantial outliers regarding generalizability of these effects (Table 8, Figure 6).
|
Study |
Outcome |
Effect Measure |
Effect Size |
95% CI Lower |
95% CI Upper |
p-value |
Weight (%) |
Heterogeneity (I²) |
|
Kwon et al. (2022) [51] |
All-cause mortality |
HR |
0.82 |
0.75 |
0.89 |
<0.01 |
50 |
50% |
|
Streppel et al. (2008) [56] |
All-cause mortality |
HR |
0.78 |
0.70 |
0.87 |
<0.001 |
50 |
50% |
|
Jenkins et al. (2003) [54] |
LDL-C |
MD |
-0.30 |
-0.45 |
-0.15 |
<0.01 |
52 |
50% |
|
Ju et al. (2022) [57] |
Blood pressure |
MD |
-3.50 |
-5.80 |
-1.20 |
<0.01 |
48 |
50% |
3. Discussion
This meta-analysis confirms and extends the existing literature that greater dietary fiber intake is significantly associated with decreased cardiovascular disease (CVD) incidence and mortality, as well as blood pressure and LDL-cholesterol. Consistent with this study pooled hazard ratios, increased fiber intake was associated with lower prevalence of cardiometabolic risk factors including obesity, hypertension and dyslipidemia from 1999–2010 National Health and Nutrition Examination Survey (NHANES) national data [26]. In addition to our findings of a protective profile of fiber specifically for cardiovascular outcomes, recent meta-analyses suggest that dietary fiber may also reduce chronic disease risk, including ovarian cancer [27], suggesting more systemic anti-inflammatory and metabolic benefits that support the overall protective effects of fiber.
Mechanistic insights go beyond epidemiological associations and support the concept that dietary fiber benefit’s vascular function. Fiber improves endothelial function and reduces oxidative stress which are the process for the atherosclerotic progression, as proposed by De Koning and Hu [28]. However, based upon our meta-analysis findings of reductions in cardiovascular events in both randomized and cohort studies, these mechanisms must underpin our results. Similar to the clinical results seen by Vuksan et al. which showed that glucomannan supplementation reduced glycemia and other risk markers in type 2 diabetes [29], we show that soluble fiber interventions, like oat bran and portfolio diets, improved glycemia. In part, these effects are attributed to prebiotic properties that induce short chain fatty acid (SCFA) production and modulate gut microbiota—an axis that is now known to play important roles in cardiovascular health [30].
Our findings are further supported by Zhang et al. [31], who observed significant inverse associations between fiber intake and atherosclerotic cardiovascular disease risk in large US cohorts; similar to our reported hazard ratios of 0.75–0.82. This is additionally upheld by reviews like in Deehan et al. [32] who saw that fiber lessened the danger of corpulence, metabolic disorder and systemic irritation (all of which are supported to CVD pathogenesis). Moreover, several reviews have demonstrated the importance of fiber in lipid metabolism. Confirming the results of Ge et al. [33] and Schoeneck and Iggman [34], fiber supplementation can significantly reduce LDL cholesterol, with reductions of up to 0.30 mmol/L in our meta-analysis. Bile acid binding and enhanced fecal cholesterol excretion enhance hepatic LDL receptor upregulation and cholesterol clearance (35; mechanistically explained here).
Similarly, our finding of a dose-responsive relationship between fiber and cardiometabolic outcomes is consistent with Yao et al. [36] who demonstrated that a 10g/day higher intake of fiber led to an approximately 9% reduction in type 2 diabetes risk. Additionally, Aleixandre and Miguel [37] found that fiber supplementation decreased mean systolic blood pressure by 3.5 mmHg (similar to our -- 3.5 mmHg change in systolic blood pressure in hypertensive adults consuming oat bran). The convergence of results in this report increases confidence in a blood pressure lowering action of dietary fiber. Weickert and Pfeiffer [38] also added that fiber improves insulin sensitivity and decreases inflammatory biomarkers, all of which would help explain our LDL and blood pressure reductions.
Fiber fermentation to produce SCFAs shown to regulate colonic Treg cell homeostasis and dampen systemic inflammation at the molecular level [39] provides a viable gut-heart immunomodulatory pathway. Also, diets high in polyunsaturated fats and fiber conspire to improve lipid profiles and lower cardiovascular risk [40] as evidenced by the consistent LDL findings and rate of CVD from our included studies.
Our conclusions are also supported by dietary pattern analyses in large cohorts (e.g., UK Biobank). According to Gao et al. [41], high-fiber dietary patterns were associated with a significantly lower risk of fatal CVD and all causes of death. The 18% to 25% reductions in mortality we observed in Kwon et al. and Streppel et al. are consistent with these results. Schulz and Slavin [42] call for developing a new paradigm of carbohydrate quality based on fiber content, charge we stand up for given that fiber has multiple health benefits displayed in our study.
However, fiber intake continues to stay below recommended levels, especially among low-income populations [43], significantly in major global studies. In the PURE study (18 countries) inverse associations between fiber intake with both blood lipids and blood pressure were demonstrated [44] and strategies to increase fiber intake remain important for public health. Even though this is the case, there are still barriers. Fiber adoption is hindered by cultural dietary preferences, food processing practice and low awareness [45].
In practice, dietary models that emphasize fiber continue to center on fiber. Both Mediterranean and DASH diets which emphasize high fiber plant foods, are consistently associated with lower CVD risk [46]. Fiber data, in turn, also show that the effects of fiber are enhanced by shifts in gut microbial composition and/or viscosity and contribute to modulating lipid and glucose metabolism [47]. Beyond our study in cardiovascular health, fiber may also protect against colorectal cancer and metabolic comorbidities [48] and other evidence is emerging. In addition, longitudinal data suggest that, in women, increased fiber intake prevents weight gain and adiposity [49], adding to the significance of this nutrient in obesity related cardiovascular risk. Based on observational data, it becomes clear that the majority of populations seldom reach 25–30g of dietary fiber daily. Thus, the World Health Organization has stressed a daily intake of 25–30g of dietary fiber as a cornerstone of a healthy diet [50].
4. Conclusion
Systematic review and meta-analysis show that greater dietary fiber intake is associated with reduced cardiovascular disease incidence, five cardiovascular deaths, blood pressure and LDL cholesterol. The protective effects are consistent from randomized trials and cohort studies and mechanism insights involving lipid metabolism, insulin sensitivity and modulation of the gut microbiota. The findings are consistent with large-scale observational studies and clinical trials cited in the broader literature, and confirm fiber's critical role in cardiometabolic health. These well documented benefits have not been sufficient to push global fiber intake up to within recommended levels. Based on this, promoting dietary fiber to prevent and manage cardiovascular disease can be considered a cost effective, evidence-based strategy that public health initiatives and clinical guidelines should forefront.
7. References
- World Health Organization (WHO): Cardiovascular Diseases (CVDs). World Health Organization. (2021).
- Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk Factors. Journal of the American College of Cardiology 74 (2019): 2529-2532.
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, et al. Heart Disease and Stroke Statistics-2018 Update: a Report from the American Heart Association. Circulation 137 (2018): e67-492.
- Pereira MA, O’Reilly E, Augustsson K, Fraser GE, Goldbourt U, et al. Dietary Fiber and Risk of Coronary Heart Disease. Archives of Internal Medicine 164 (2004): 370.
- Mcrorie JW, Fahey GC. A review of gastrointestinal physiology and the mechanisms underlying the health benefits of dietary fiber: Matching an effective fiber with specific patient needs. Clinical Nursing Studies 1 (2013).
- Slavin JL. Dietary Fiber and Body Weight. Nutrition 21 (2005): 411-418.
- Jones JM. Dietary Fiber Future Directions: Integrating New Definitions and Findings to Inform Nutrition Research and Communication. Advances in Nutrition 4 (2013): 8-15.
- Reynolds A, Mann J, Cummings J, Winter N, Mete E. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet 393 (2019): 434-445.
- Weickert MO, Pfeiffer AFH. Metabolic Effects of Dietary Fiber Consumption and Prevention of Diabetes. The Journal of Nutrition 138 (2008): 439-442.
- InterAct Consortium. Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct Study and a meta-analysis of prospective studies. Diabetologia 58 (2015): 1394-1408.
- Gunness P, Gidley MJ. Mechanisms underlying the cholesterol-lowering properties of soluble dietary fibre polysaccharides. Food & Function 1 (2010): 149.
- Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, et al. Beneficial Effects of High Dietary Fiber Intake in Patients with Type 2 Diabetes Mellitus. New England Journal of Medicine 342 (2000): 1392-1398.
- Soliman GA. Dietary Fiber, Atherosclerosis, and Cardiovascular Disease. Nutrients 11 (2019): 1155.
- Hedner T, Narkiewicz K, Oparil S, Kjeldsen SE. Primary cardiovascular prevention by Mediterranean diet – The PREDIMED trial. Blood Pressure 22 (2013): 129-130.
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. The New England Journal of Medicine 344 (2001): 3-10.
- Hopkins PN. Effects of dietary cholesterol on serum cholesterol: a meta-analysis and review. The American Journal of Clinical Nutrition 55 (1992): 1060-1070.
- Reyna-Villasmil N, Bermúdez-Pirela V, Mengual-Moreno E, Arias N, Cano-Ponce C, et al.: Oat-derived β-Glucan Significantly Improves HDLC and Diminishes LDLC and Non-HDL Cholesterol in Overweight Individuals With Mild Hypercholesterolemia. American Journal of Therapeutics 14 (2007): 203-212.
- Trumbo P, Schlicker S, Yates AA, Poos M. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. Journal of the American Dietetic Association 102 (2002): 1621-1630.
- McGill C, III V, Devareddy L. Ten-Year Trends in Fiber and Whole Grain Intakes and Food Sources for the United States Population: National Health and Nutrition Examination Survey 2001–2010. Nutrients 7 (2015): 1119-1130.
- Howarth NC, Saltzman E, Roberts SB. Dietary Fiber and Weight Regulation. Nutrition Reviews 59 (2009): 129-139.
- Slavin J: Fiber and Prebiotics: Mechanisms and Health Benefits. Nutrients. 5 (2013): 1417-1435.
- Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F: From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell 165 (2016): 1332-1345.
- Kaczmarczyk MM, Miller MJ, Freund GG: The health benefits of dietary fiber: Beyond the usual suspects of type 2 diabetes mellitus, cardiovascular disease and colon cancer. Metabolism 61 (2012): 1058-1066.
- Threapleton DE, Greenwood DC, Evans CEL, Cleghorn CL, Nykjaer C, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ 347 (2013): f6879-9.
- Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary Intake Among US Adults, 1999-2012. JAMA 315 (2016): 2542.
- Grooms KN, Ommerborn MJ, Pham DQ, Djoussé L, Clark CR. Dietary Fiber Intake and Cardiometabolic Risks among US Adults, NHANES 1999-2010. The American Journal of Medicine 126 (2013):1059-1067.
- Zheng B, Shen H, Han H, Han T, Qin Y. Dietary fiber intake and reduced risk of ovarian cancer: a meta-analysis. Nutrition Journal 17 (2018).
- de Koning L, Hu FB. Do the Health Benefits of Dietary Fiber Extend Beyond Cardiovascular Disease? Archives of Internal Medicine 171 (2011): 1069.
- Vuksan V, Jenkins DJ, Spadafora P, Sievenpiper JL, Owen R, et al. Konjac-mannan (glucomannan) improves glycemia and other associated risk factors for coronary heart disease in type 2 diabetes. A randomized controlled metabolic trial. Diabetes Care 22 (1999): 913-919.
- Bindels LB, Delzenne NM, Cani PD, Walter J. Towards a more comprehensive concept for prebiotics. Nature Reviews Gastroenterology & Hepatology 12 (2015): 303-310.
- Zhang S, Tian J, Lei M, Zhong C, Zhang Y. Association between dietary fiber intake and atherosclerotic cardiovascular disease risk in adults: a cross-sectional study of 14,947 population based on the National Health and Nutrition Examination Surveys. BMC Public Health 22 (2022).
- Deehan EC, Mocanu V, Madsen KL. Effects of dietary fibre on metabolic health and obesity. Nature Reviews Gastroenterology & Hepatology 21 (2024): 1-18.
- Ge Q, Yan Y, Luo Y, Teng T, Cao C, et al. Dietary supplements: clinical cholesterol-lowering efficacy and potential mechanisms of action. International Journal of Food Sciences and Nutrition 75 (2024): 349-368.
- Schoeneck M, Iggman D. The effects of foods on LDL cholesterol levels: A systematic review of the accumulated evidence from systematic reviews and meta-analyses of randomized controlled trials. Nutrition, Metabolism and Cardiovascular Diseases 31 (2021): 1325-1338.
- Graham MJ, Lemonidis KM, Whipple CP, Subramaniam A, Monia BP, et al. Antisense inhibition of proprotein convertase subtilisin/kexin type 9 reduces serum LDL in hyperlipidemic mice. Journal of Lipid Research 48 (2007): 763-767.
- Yao B, Fang H, Xu W, Yujie Yan, Huilin Xu, et al. Dietary fiber intake and risk of type 2 diabetes: a dose–response analysis of prospective studies. European Journal of Epidemiology 29 (2014): 79-88.
- Aleixandre A, Miguel M. Dietary fiber and blood pressure control. Food & Function 7 (2016): 1864-1871.
- Weickert MO, Pfeiffer AF. Impact of dietary fiber consumption on insulin resistance and the prevention of type 2 diabetes. The Journal of Nutrition 148 (2018): 7-12.
- Smith PM, Howitt MR, Panikov N, et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 341 (2013): 569-573.
- Virtanen JK. Dietary polyunsaturated fat intake in coronary heart disease risk. Clinical Lipidology 10 (2015): 115-117.
- Gao M, Jebb SA, Aveyard P. Associations between dietary patterns and the incidence of total and fatal cardiovascular disease and all-cause mortality in 116,806 individuals from the UK Biobank: a prospective cohort study. BMC Medicine 19 (2021).
- Schulz R, Slavin J. Perspective: defining carbohydrate quality for human health and environmental sustainability. Advances in Nutrition 12 (2021).
- Virani SS, Alonso A, Benjamin EJ. Heart disease and stroke statistics 2020 update. Circulation 141 (2020).
- Mente A, Dehghan M, Rangarajan S. Association of dietary nutrients with blood lipids and blood pressure in 18 countries: a cross-sectional analysis from the PURE study. The Lancet Diabetes & Endocrinology 5 (2017): 774-787.
- Ozdemir O. Prebiotics and probiotics in allergy: potential mechanisms of prebiotics’ and probiotics’ actions in allergy - (Part 1). MOJ Immunology 3 (2016).
- Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet. Circulation 123 (2011): 2870-2891.
- Li Y, Xia D, Chen J. Dietary fibers with different viscosity regulate lipid metabolism via AMPK pathway: roles of gut microbiota and short-chain fatty acid. Poultry Science 101 (2022): 101742.
- Murphy N, Norat T, Ferrari P. Dietary fibre intake and risks of cancers of the colon and rectum in the European Prospective Investigation into Cancer and Nutrition (EPIC). PLoS ONE 7 (2012): e39361.
- Tucker LA, Thomas KS. Increasing total fiber intake reduces risk of weight and fat gains in women. The Journal of Nutrition 139 (2009): 576-581.
- World Health Organization. Healthy diet. World Health Organization (2020).
- Kwon YJ, Lee HS, Park G, Kim HM, Lee JW. Association of dietary fiber intake with all-cause mortality and cardiovascular disease mortality: a 10-year prospective cohort study. Nutrients 14 (2022): 3089.
- Lairon D, Arnault N, Bertrais S, Planells R, Clero E, et al. Dietary fiber intake and risk factors for cardiovascular disease in French adults. The American Journal of Clinical Nutrition 82 (2005): 1185-1194.
- Mozaffarian D. Cereal, fruit, and vegetable fiber intake and the risk of cardiovascular disease in elderly individuals. JAMA 289 (2003): 1659.
- Jenkins DJA. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA 290 (2003): 502.
- Keogh JB, Brinkworth GD, Noakes M, Belobrajdic DP, Buckley JD, et al. Effects of weight loss from a very-low-carbohydrate diet on endothelial function and markers of cardiovascular disease risk in subjects with abdominal obesity. The American Journal of Clinical Nutrition 87 (2008): 567-576.
- Streppel MT, Ocké MC, Boshuizen HC, Kok FJ, Kromhout D. Dietary fiber intake in relation to coronary heart disease and all-cause mortality over 40 y: the Zutphen Study. The American Journal of Clinical Nutrition 88 (2008): 1119-1125.
- Ju Y, Zhang C, Zhang Z. Effect of dietary fiber (oat bran) supplement in heart rate lowering in patients with hypertension: a randomized DASH-diet-controlled clinical trial. Nutrients 14 (2022): 3148.
- Buil-Cosiales P, Toledo E, Salas-Salvadó J. Association between dietary fibre intake and fruit, vegetable or whole-grain consumption and the risk of CVD: results from the PREvención con DIeta MEDiterránea (PREDIMED) trial. British Journal of Nutrition 116 (2016): 534-546.
© 2016-2025, Copyrights Fortune Journals. All Rights Reserved